Surgical anatomy of the trachea
Introduction
The surgeon’s mastery of anatomy is paramount to performing a successful operation and, thus, to improving the life of the patient. This, however, does not merely entail the memorization of structures and their placement in two-dimensions. The practicing surgeon must understand the relationship between structures in real space and anticipate common variations in those structures at the time of dissection (1). Surgical anatomy also respects the biology and function of structures in the operative field, appreciates the consequences of altering the arrangement of those structures, and must account for the distorting effect of pathology on a structure or a neighboring structure. For the tracheal surgeon, these principles certainly hold true, as airway complications can be highly morbid and quickly fatal.
Structure of the trachea
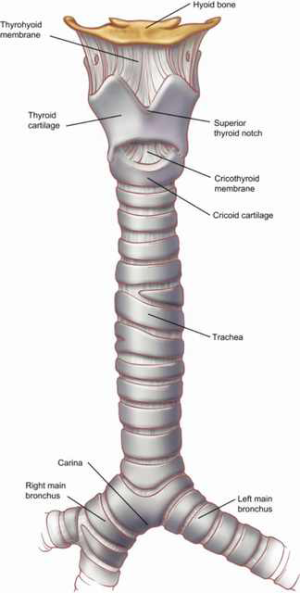
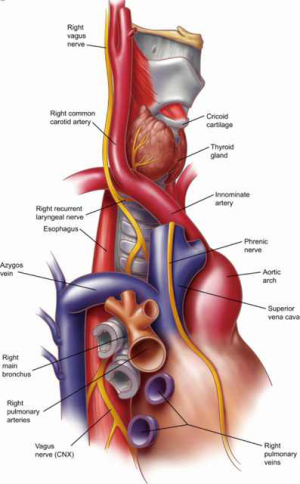
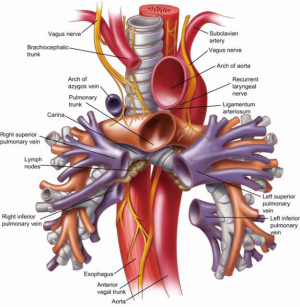
The trachea is a conduit between the outside world and the parenchyma of the lungs. Oxygen from the atmosphere travels to the lungs during inspiration and carbon dioxide is ventilated from the lungs to the atmosphere during expiration. The trachea is a cartilaginous tubular structure connecting the larynx superiorly and the main bronchi inferiorly (Figure 1) (2). The lower edge of the cricoid cartilage defines the beginning of the trachea. The end of the trachea is marked by the carina, the steep-angled take off of the right main bronchus, and the take off of the more horizontal left main bronchus. The carina is usually found at the level of the T4 vertebral body but its vertical position in the mediastinum changes with the phases of respiration. On average, the length of the trachea is 11.8 cm with a normal range of 10 to 13 cm in males. The trachea tends to be shorter in females.
In the adult, the trachea sits anteriorly in the neck and dives posteriorly in the mediastinum as it travels toward the carina. This angle of descent is more acute in children and tends to become more horizontal with age due to kyphotic changes in the spine and tethering of the left main stem bronchus under the aortic arch. This age-related change needs to be considered when assessing and positioning a patient for tracheostomy placement, in elderly patients the length of the trachea in the neck tends to remain constant with cervical extension, this contrasts with younger patients for whom it tends to lengthen.
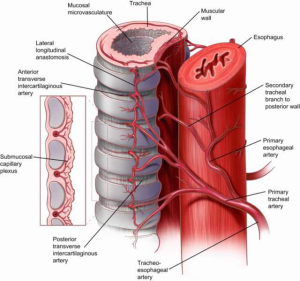
The scaffolding of the trachea is comprised of 18 to 22 D-shaped “rings” with anterior and lateral walls made of C-shaped cartilage and a posterior membranous wall connecting the arms of the C (Figure 2). The trachealis muscle runs longitudinally on the posterior aspect of this wall and abuts the anterior esophagus. An intercartilaginous membrane connects the inferior edge of the upper cartilage to the superior edge of the cartilage below. There are approximately two rings of cartilage per centimeter of trachea and each tracheal ring is an average of 4 mm in height. The wall of the trachea averages about 3 mm in thickness. The average external diameter of the trachea is 2.3 and 1.8 cm in the coronal and sagittal dimensions, respectively.
At birth, the cross-sectional shape of the tracheal lumen is circular. As a child grows into an adult, the lumen most commonly takes on an ovoid form, though a persistent circular shape is a normal adult variant. The luminal diameter of the trachea varies with alterations in intraluminal pressure occurring during normal respiration, ventilation and Valsalva maneuvers. Coughing narrows the lumen by causing the trachealis muscle of the posterior wall to pull the cartilaginous C-arms together. With age or obstructive airway disease, the lateral diameter of the lumen tends to narrow, while the anteroposterior (AP) diameter increases, resulting in the “saber sheath” trachea. The walls of this tracheal formation may exhibit wall calcification. Ring softening in chronic obstructive pulmonary disease results in AP narrowing of the lumen in the setting of posterior wall thickening. This can cause luminal obstruction during expiration or coughing.
The luminal mucosa of the trachea is lined by ciliated pseudostratified columnar epithelium containing mucous producing goblet cells. The mucosa also harbors ducts that connect mucous glands in the submucosa to the surface of the tracheal lumen. The surface mucous and cilia act in partnership to trap and expel particulates or microorganisms that enter the airway. Airborne irritants can temporarily or permanently damage this mucociliary escalator. Long-term cigarette smokers, for example, have increased mucous production and defective ciliary function, making them dependent on an effective cough to clear their airways.
Blood supply to the trachea
Safe and successful tracheal dissection demands a detailed understanding of tracheal blood supply to avoid the sequelae of tracheal ischemia (e.g., tracheal stenosis and anastomotic breakdown). A fundamental principle that the airway surgeon must always bear in mind is that the arteries feeding the trachea approach the tracheal wall laterally and vascularize the trachea in a segmental fashion along its longitudinal access (Figure 2). As the various segmental arteries supplying the trachea approach the lateral tracheal wall, they branch superiorly and inferiorly in a longitudinal fashion forming anastomoses with the segmental arteries above and below. Within the intercartilaginous ligaments the tracheal arteries again branch into anterior and posterior branches that travel circumferentially within the tracheal wall where they anastomose with the corresponding tracheal arteries from the contralateral side. This segmental arrangement of blood flow limits circumferential tracheal dissection to no more than 1–2 cm on either side of a tracheal anastomosis due to the risk of devascularization and ischemia with larger dissections.
The arterial supply of the trachea divides it into the upper (cervical) and lower (thoracic) trachea. The tracheoesophageal branches of the inferior thyroid arteries bring blood to the cervical trachea from the right and left thyrocervical trunks that branch off the subclavian arteries (Figure 3). While the configuration of the branches may vary slightly between individuals, in general, the first tracheoesophageal branch supplies the lower cervical trachea, the second branch supplies the middle cervical trachea and the third branch supplies the upper cervical trachea. The superior thyroid artery does not directly supply the trachea but forms an anastomosis with the inferior thyroid artery where fine branches supply the thyroid isthmus and the adjacent anterior tracheal wall.
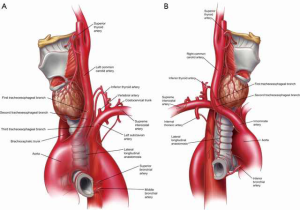
The thoracic trachea and carina receive blood from the bronchial arteries arising directly from the aorta (Figure 3). Most commonly, there is a superior, middle and inferior bronchial arteries responsible for bringing blood to the trachea and carina. The superior bronchial artery comes off the anteromedial aspect of the descending thoracic aorta lateral to the carina and posterior to the left main bronchus. Its anterior branch courses over the proximal left main stem bronchus, which it supplies on its way to providing blood to the anterior portion of the carina. The principal and posterior branches of the superior bronchial artery pass behind the posterior wall of the esophagus to supply the proximal right main stem bronchus. Any number of these branches may arise from an intercostal bronchial trunk. The middle bronchial artery comes off the aorta distal to the superior bronchial artery and travels posterior to the medial aspect of the left main stem bronchus to supply the carina as it anastomoses with the anterior branch of the superior bronchial artery or higher tracheoesophageal branches. The inferior bronchial artery arises off the right posteromedial ascending thoracic aorta to supply the left main stem bronchus. Though the patterns of bronchial artery branching are highly varied, approximately 40% of the time the left bronchial tree receives blood from two left-sided aortic branches and the right main stem bronchus is supplied by one right-sided aortic branch.
Structural relationships with the trachea
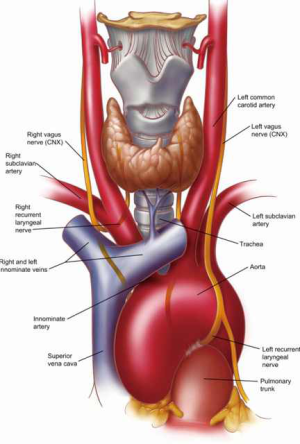
The right and left lobes of the thyroid gland sit anterolateral to the proximal cervical trachea and the isthmus connecting the two lobes tends to cross the anterior trachea at the 2nd or 3rd tracheal ring (Figure 4). In addition to the proximal trachea, the inferior thyroid artery provides blood to the inferior thyroid gland.
The esophagus has an intimate relationship with the trachea along its course (Figures 2 and 3B). The esophagus begins at the level of the cricoid cartilage and runs toward the gastroesophageal junction along the left posterior border of the trachea. Fibroelastic membranes and rare muscle fibers lie between the longitudinal muscle of the outer esophagus and the trachealis muscle. The right posterior border of the trachea runs along the anterior aspect of the vertebral bodies. Occasionally, the esophagus may be found more laterally on the left side making it prone to injury during mediastinoscopy.
The right and left vagus nerves travel distally through the neck in a position posterolateral to the corresponding common carotid arteries (Figure 4). The right and left recurrent laryngeal nerves are branches of the vagus nerves and function to innervate the true vocal cords. They enter the larynx between the thyroid and cricoid cartilages under the inferior horn, or cornua, of the thyroid cartilage. The origin of the left recurrent laryngeal nerve occurs distal to the aortic arch when it then dives and courses posteromedially just lateral to the ligamentum arteriosum, at which point it recurs and ascends toward the cricoid cartilage within the left tracheoesophageal groove. The right recurrent laryngeal nerve branches off the right vagus nerve just distal to the right subclavian artery when its course then dives posteromedially under the origin of the right subclavian where it recurs and ascends toward the cricoid cartilage in the right tracheoesophageal groove. A non-recurrent laryngeal nerve variant running from the vagus nerve at the level of the thyroid cartilage directly to the larynx is seen in 0.5–0.7% of patients. Injury to the recurrent laryngeal nerves, whether by complete or partial transection, traction, contusion, thermal burn, ischemia or tumor invasion, can cause vocal cord paresis or paralysis resulting in hoarseness or complete loss of voice or airway depending on the extent of injury and the integrity of the contralateral nerve. The thoracic surgeon must respect the course of these nerves during dissection of the proximal trachea.
There are a number of large blood vessels lying in close proximity to the trachea that must be respected during tracheal operations. The brachiocephalic, or innominate, artery is the first branch of the aortic arch (Figure 4). It originates at the right anterior aspect of the trachea and runs superiorly from left-to-right over the right anterolateral portion of the distal and mid trachea. The left common carotid artery is the next branch of the aorta. It takes off just to the left of the trachea’s midline and runs superiorly from right-to-left over the left anterolateral trachea. The superior vena cava courses toward the right atrium along the right anterior aspect of the trachea (Figure 5). The azygous vein, coursing superiorly along the right side of the thoracic vertebral column before bending anteriorly, joins the superior vena cava lateral and just superior to the right tracheobronchial angle. Care must be taken during mediastinoscopy to anticipate this landmark so as to avoid mistaking the azygos vein for a lymph node during biopsy.
The main pulmonary artery, or pulmonary trunk, lies anterior and to the left of the carina (Figure 6). Its branches, the right and left pulmonary artery, run laterally and anterior to their corresponding main stem bronchi before branching into the lobar arteries of the right and left lungs. The positioning of the pulmonary arteries in relationship to the main stem bronchi must be remembered when mobilization of the subcarinal and tracheobronchial lymph nodes is attempted during mediastinoscopy. Additionally, excessive traction on the right-sided lower paratracheal nodes risks massive blood loss, as these nodes are in close proximity to the first branch of the right pulmonary artery. A review of the regional lymph node maps for lung cancer screening is beyond the scope of this article, but all thoracic surgeons should understand the key anatomic relationships and clinical significance of various node stations found along the trachea, carina and bronchi.
This article provides a solid foundation in the anatomy of the trachea and its relationship with critical mediastinal structures. A surgeon’s mastery of this material supports safe and effective operative planning and allows for the anticipation of common anatomical variations, thereby reducing patient morbidity and mortality in the operating room. In addition, the development of new surgical techniques that promise to improve patient outcomes is dependent on a deep respect for the human anatomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.