Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.3082
Peer-review started: April 20, 2020
First decision: June 2, 2020
Revised: June 16, 2020
Accepted: July 1, 2020
Article in press: July 1, 2020
Published online: July 26, 2020
Pulmonary benign metastatic leiomyoma (PBML), which is very rare, is a type of benign metastatic leiomyoma (BML). Here, we report a case of PBML, finally diagnosed through multidisciplinary team (MDT) discussions, and provide a literature review of the disease.
A 55-year old asymptomatic woman was found to have bilateral multiple lung nodules on a chest high-resolution computed tomography (HRCT) scan. Her medical history included total hysterectomy for uterine leiomyoma. The patient was diagnosed with PBML, on the basis of her clinical history, imaging manifestations, and computed tomography (CT)-guided percutaneous lung puncture biopsy, via MDT discussions. As the patient was asymptomatic, she received long-term monitoring without treatment. A follow-up of chest HRCT after 6 mo showed that the PBML lung nodules were stable and there was no progression.
For patients with a medical history of hysterectomy and uterine leiomyoma with lung nodules on chest CT, PBML should be considered during diagnosis based on the clinical history, imaging manifestations, CT-guided percutaneous lung puncture biopsy, and MDT discussions.
Core tip: Pulmonary benign metastatic leiomyoma (PBML) is a rare disease, and a type of benign metastatic leiomyoma, which is usually misdiagnosed. In order to avoid misdiagnosis and treat this disease effectively, we report the diagnosis and treatment of a patient with PBML as the final diagnosis based on her clinical history of uterine leiomyoma, imaging manifestations, biopsy, and multidisciplinary team discussions. A literature review of PBML was also carried out.
- Citation: Dai HY, Guo SL, Shen J, Yang L. Pulmonary benign metastasizing leiomyoma: A case report and review of the literature. World J Clin Cases 2020; 8(14): 3082-3089
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/3082.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.3082
Pulmonary benign metastatic leiomyoma (PBML) is a type of benign metastatic leiomyoma (BML) that was first reported in 1939[1]. The etiology of PBML is related to uterine leiomyoma, and PBML mainly occurs in premenopausal women who have received a myomectomy or hysterectomy, but there are also cases of this disease occurring in women who have not received surgery, as well as in men and children[2,3]. Typically, the appearance of PBML on imaging is multiple nodules of different sizes in the bilateral lungs, such as in our case. There are also cases that have single or unilateral lung nodules. PBML is considered benign in histopathology, but the fusiform smooth muscle cells of the uterus can be diffused by metastasis, so it is likely that the biological behavior of PBML has also been considered malignant. BML often involves the lungs, as in our case of PBML, but it may also involve the heart, skeletal system, vascular system, lymph nodes, or other organs and systems. In the described case, multiple lung nodules were found. However, most PBML patients have no clinical manifestations, while some have hemoptysis, chest pain, dyspnea, pneumothorax, or other presentations. Surgery and anti-estrogen therapy can be considered for the treatment of PBML. Although, for patients without symptoms and progression, only follow-up observation is needed, as PBML generally has a good prognosis.
A 55-year-old asymptomatic Chinese woman was found to have multiple nodules in both lungs during a health checkup.
No symptoms present.
Her medical history included total hysterectomy for uterine leiomyoma 14 years previously.
She was a non-smoker without relevant family history or recent weight loss.
She had no obvious abnormalities on physical examination.
Lung cancer tumor marker was normal, and other auxiliary examination results were unremarkable.
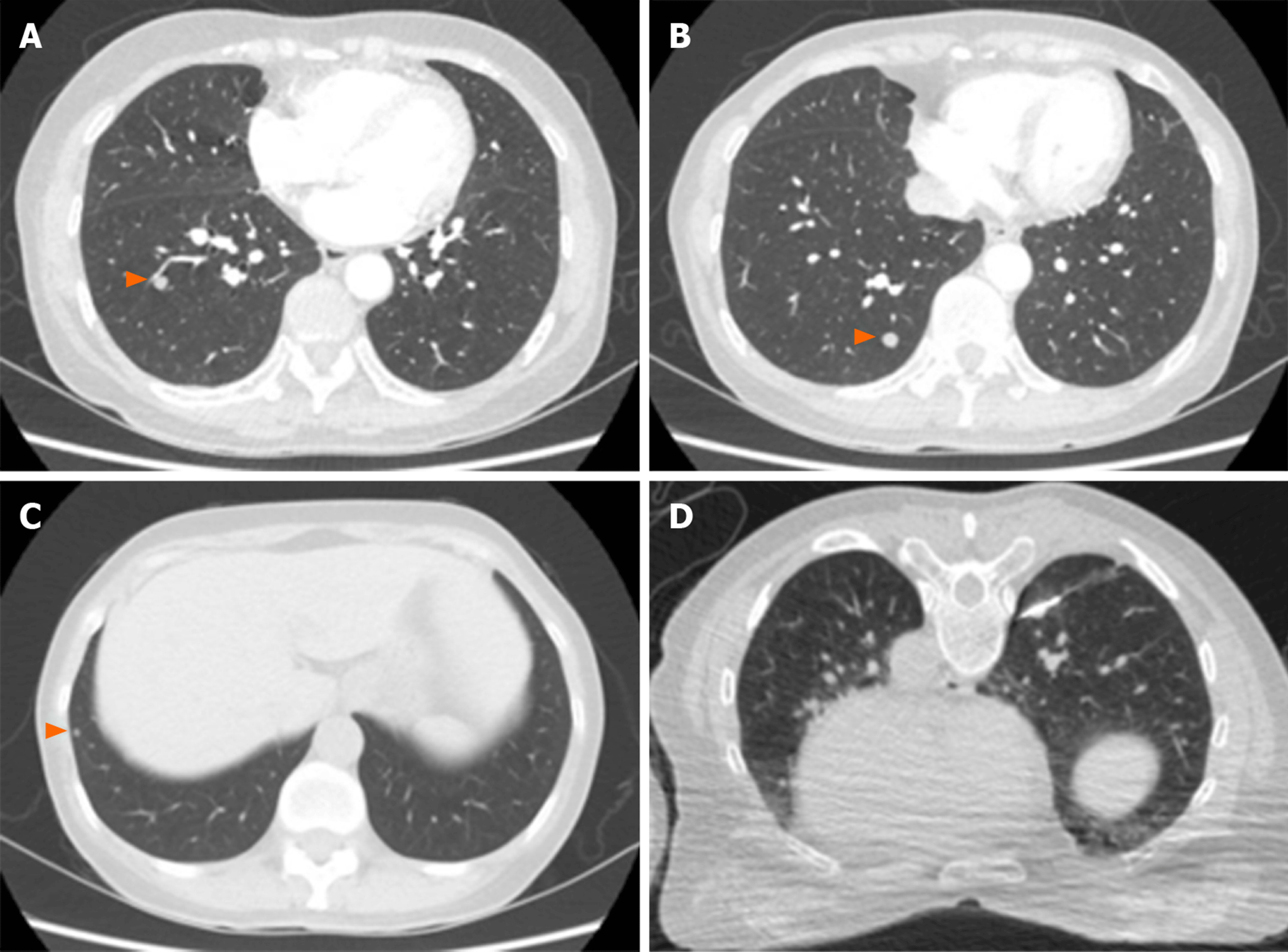
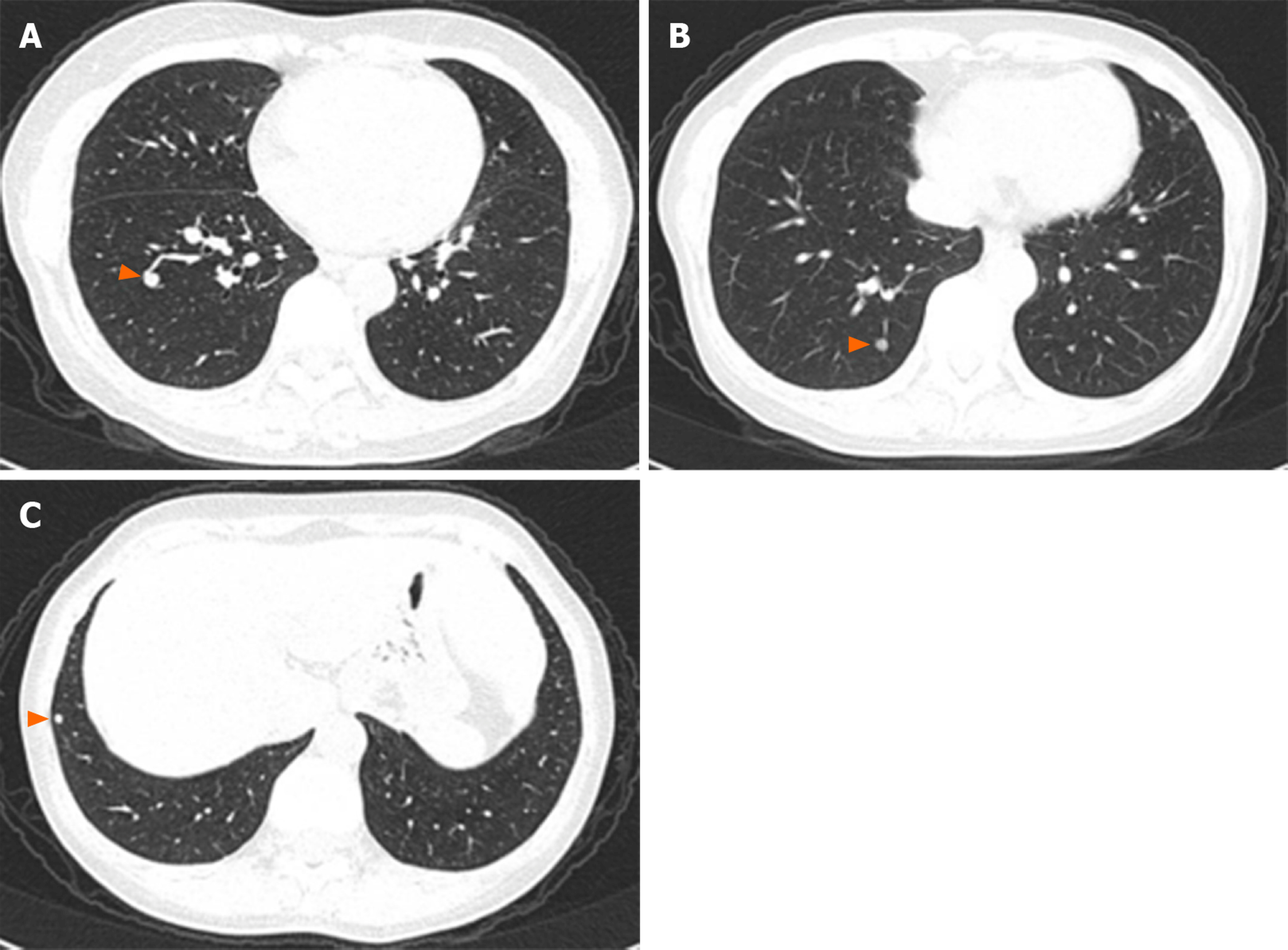
On a chest high-resolution computed tomography (HRCT) scan (Figure 1A-C), the largest nodule of 7 mm in diameter was detected in the right lower lobe.
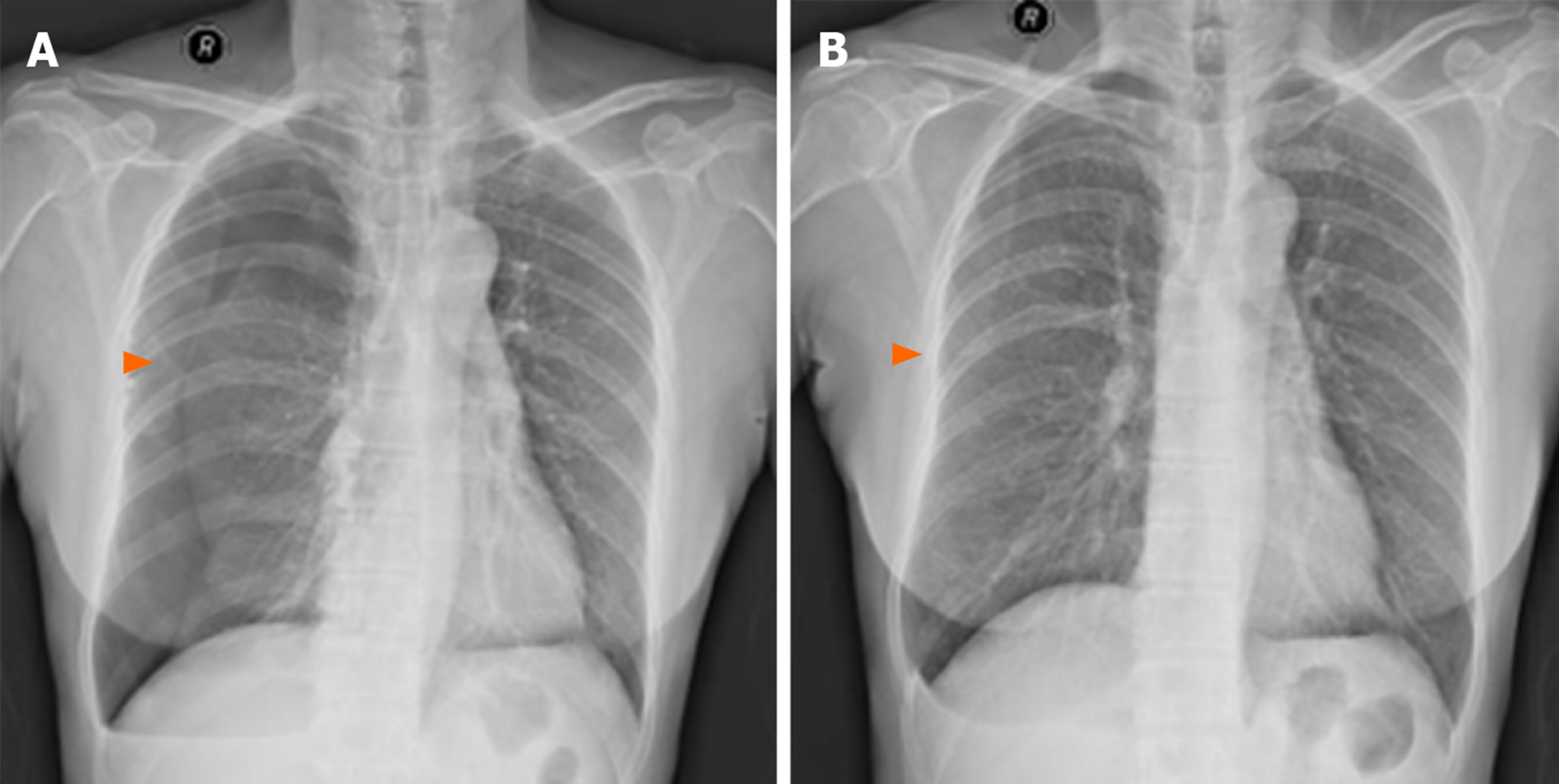
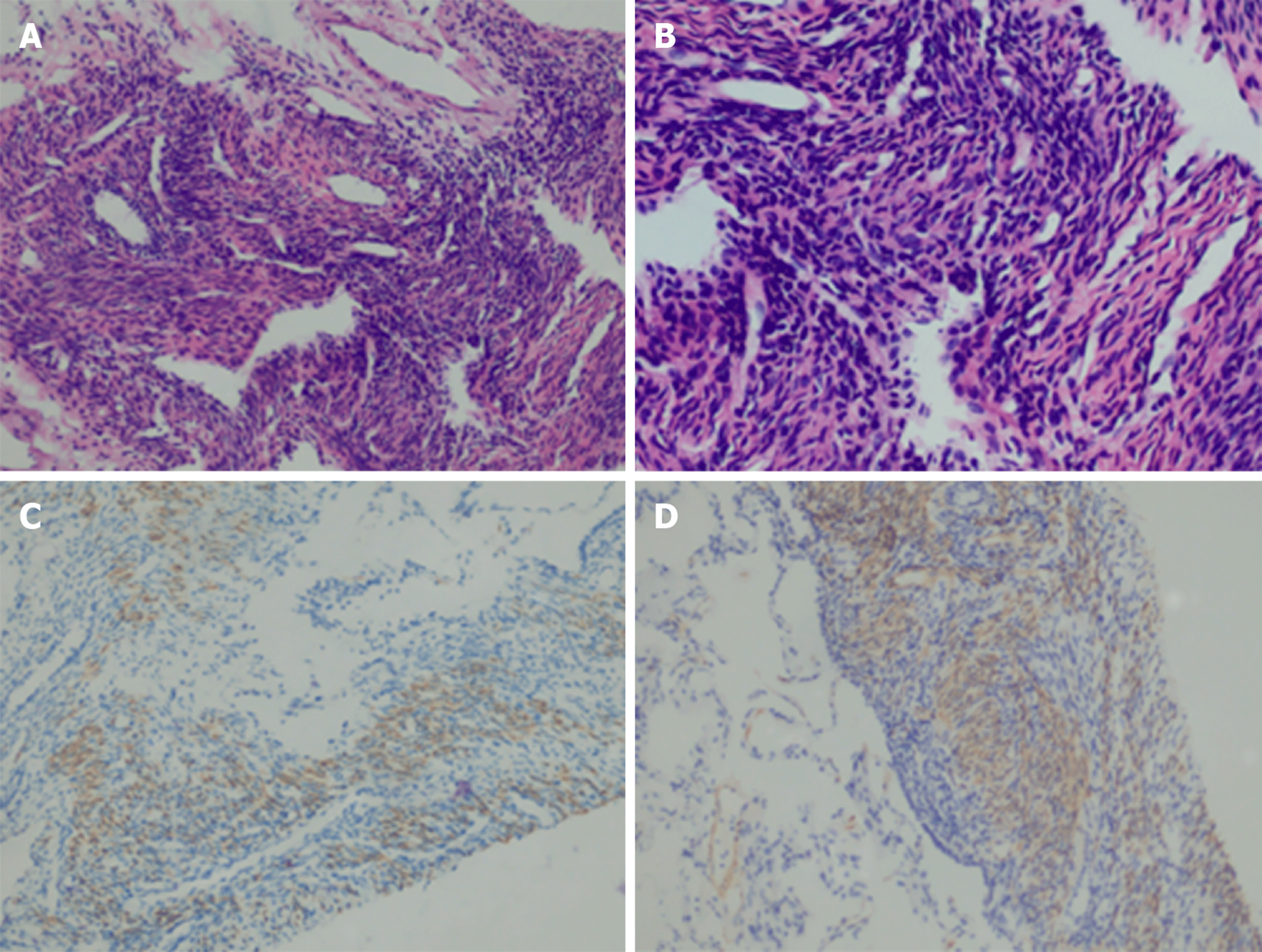
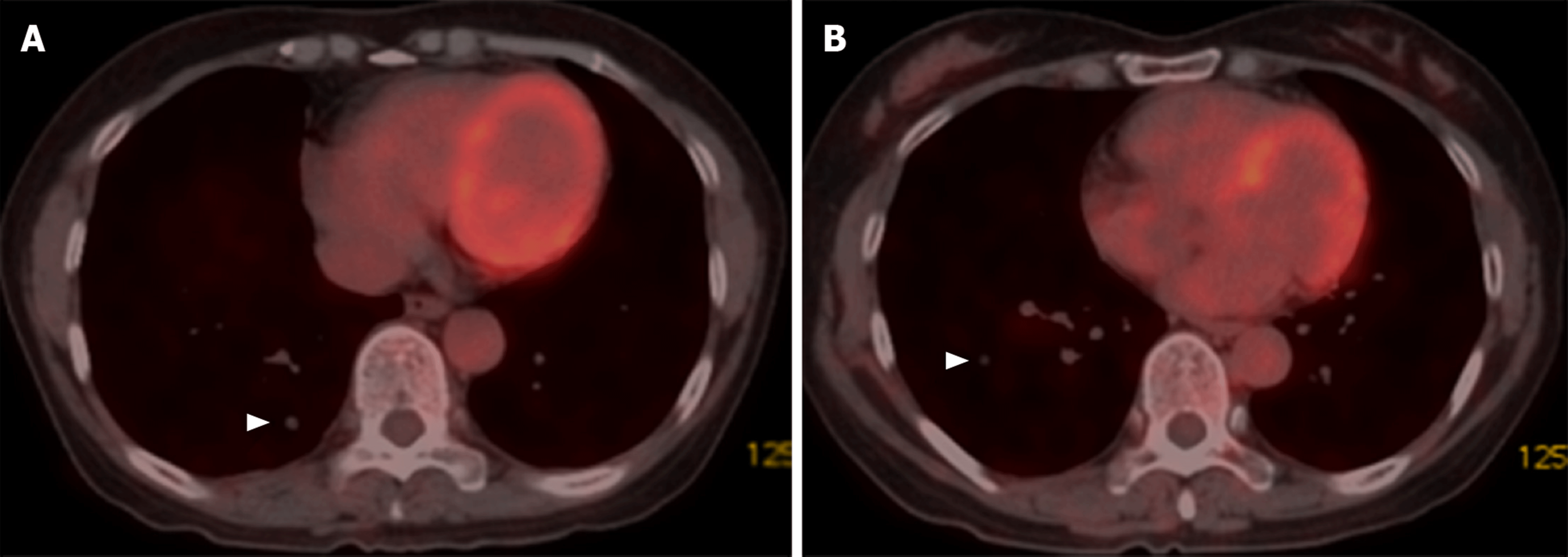
Lung cancer metastasis or metastatic lung cancer was suspected, and she was admitted to our department. Following informed consent, she underwent a computed tomography (CT)-guided percutaneous lung puncture biopsy (Figure 1D) with pneumothorax complication (Figure 2A), and recovered after thoracic puncture and aspiration (Figure 2B). Her lung puncture biopsy smear found neither cancer cells nor tuberculosis. Histopathological examination of a lung puncture biopsy specimen of the largest nodule in the right lower lobe showed the following manifestations (Figure 3A-D): A few spindle cells (spindle cell tumor was considered); and immuno-histochemistry results of Desmin(+), CD34 blood vessel(+), Bc1-2(+), SMA(+), Vim(+), S-100(-), CD99(+), STAT-6(-), and CR(-). The immunohistochemical smooth-muscle markers SMA and Desmin were positive, suggesting the origin was smooth muscle; however, because Bcl-2 and CD99 showed positive staining, a synovial origin was not excluded. Positron emission tomography-CT (PET-CT) (Figure 4A, 4B) showed multiple nodules in both lungs and no uptake of fluorodeoxyglucose (FDG), which is usually taken up by tumor lesions; there were no suspicious tumor lesions elsewhere on PET-CT.
After a multidisciplinary team (MDT) discussion, which involved personnel from six hospital departments (respiratory, oncology, obstetrics and gynecology, imaging, pathology, and nuclear medicine) and comprehensive consideration of past history, clinical manifestations, and histopathological results, the patient was finally diagnosed with PBML from uterine leiomyoma.
Because her lesions were small and she had no symptoms, she received follow-up monitoring without treatment.
Six months later, she underwent chest HRCT (Figure 5A-C), which showed no progression.
PBML is a rare disease, with only around 100 cases reported worldwide. In 2006, Pacheco-Rodriguez et al[4] reviewed the current knowledge on BML. Research papers and case reports on PBML before and after 2006 have been collated for this literature review.
The etiology of PBML is still unclear, but there are three main hypotheses: (1) The mainstream hypothesis states that after myomectomy or hysterectomy, smooth muscle cells are transported through blood and lymph vessels to the lungs and other sites (“transport theory”). But this hypothesis does not explain why non-surgical patients also develop PBML. The study performed by Patton et al[5] showed positive expression of estrogen receptor (ER) and progesterone receptor (PR) in PBML tissue, which supports the hypothesis that PBML is transferred from uterine fibroids to the lungs; (2) The second hypothesis is that PBML metastasizes to other organs and systems because it is a low grade, malignant, and highly differentiated leiomyosarcoma[6]; and (3) Others have hypothesized that PBML has multifocal origins, as some PBMLs have been found before or at the same time as uterine fibroids. Thus, in this hypothesis, PBML is considered a multiple smooth muscle hamartoma, not a metastasis[7].
Pathologically, PBML may present as an extrauterine smooth-muscle cell proliferation[8,9], and, as seen in our case, with a few spindle cells on histopathological examination. Uterine smooth muscle cells express ER and PR, as do PBML cells[8]. Cells of PBML have a low mitotic index; therefore, PBML nodules grow slowly and may remain unchanged for a long time. Cells have no nuclear atypia and necrosis, and no invasion to the surrounding tissue, while BML cells can destroy the lumbar vertebrae; therefore, some people believe that the biological behavior of PBML is malignant[10]. As shown in our case, PBML is often immunohistochemically positive for the typical muscle-cell markers SMA and Desmin.
As in the described case, PBML patients are often asymptomatic, and almost 30% of PBML patients have pulmonary manifestations, such as dyspnea, cough, and chest pain. Moreover, pneumothorax and cysts may occur in PBML patients, who should be differentially diagnosed for lymphangioleiomyomatosis (LAM), as this disease has the clinical characteristics of recurrent pneumothorax and cysts[11]. Rarely, PBML can cause respiratory failure[12] and present as progressive pneumothorax[13]. In addition, BML can affect other organs and systems in PBML patients; therefore, other systems may manifest clinical symptoms, such as leg aches and paresthesia due to spinal BML[14]. Uterine leiomyoma itself could result in gynecological symptoms, including abnormal uterine bleeding and pelvic pressure or pain.
With regard to imaging, chest X-ray, CT, 18F-fluorodeoxyglucose-PET/CT (18F-FDG-PET/CT), and magnetic resonance imaging can be used to investigate PBML. Usually, as in our case, the imaging results show pulmonary abnormalities, and multiple well-circumscribed nodules in the bilateral pulmonary fields are characteristic manifestations of chest CT[15]. The nodules may vary in size and can also be solitary or multiple but only affect one lung. Rarely, PBML presents as diffuse miliary lesions in the lungs. The nodules are mostly solid with no calcification but can also be cavitated[16-19]; the edges are smoother and clearer without enhancement than those of general malignant metastasis but may also be lobulated and enhanced on contrast-enhanced CT[10]. On 18F-FDG-PET/CT, most pulmonary nodules of PBML show low or no metabolic activity, as in our case; therefore, 18F-FDG-PET/CT may be used to differentiate PBML from malignant metastases. A case reported by Sawai et al[20] showed that metastatic lesions had high metabolic activity with maximum standard uptake values of 20.1, which is the same as the value for the diagnosis of pulmonary nodules. HRCT is more sensitive for the diagnosis of small PBML lesions.
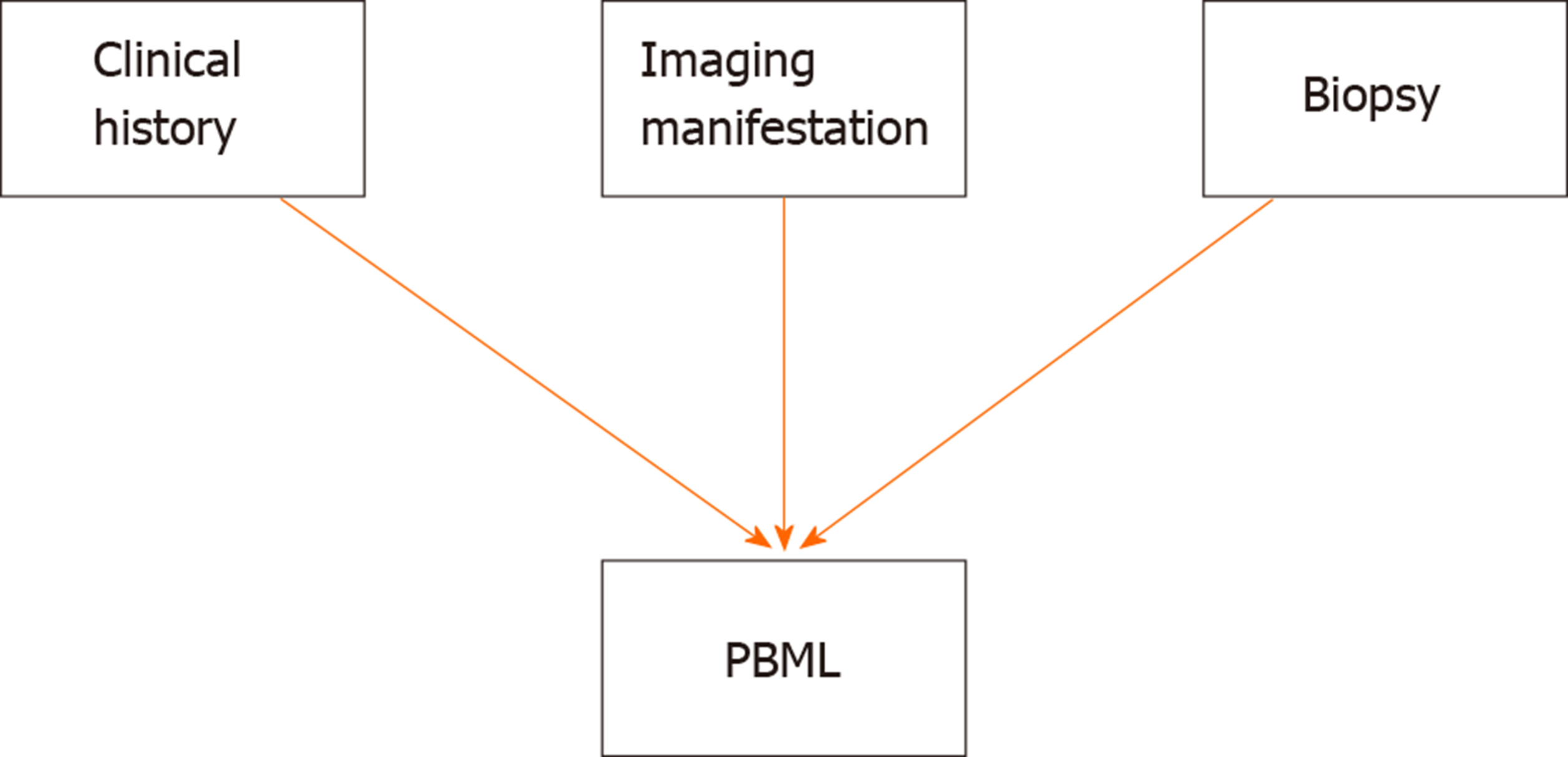
There are no standardized diagnostic criteria for PBML. PBML is diagnosed by three major aspects (Figure 6): The clinical history (history of prior hysterectomy or myomectomy); Imaging manifestations (most significant diagnostic stage); Biopsies (CT-guided percutaneous lung puncture biopsy, bronchial biopsy, surgical lung biopsy); and Histopathological evaluation (uterine leiomyoma-like spindle-shaped cells, smooth muscle markers on immunohistochemistry, ER, and PR). However, these three aspects sometimes show atypical manifestations. In such cases, an MDT, mostly involving specialists from respiratory, oncology, obstetrics and gynecology, imaging, pathology, and nuclear medicine fields, is needed to diagnose PBML. The differential diagnosis of PBML, mainly includes diseases that manifest as diffuse multiple pulmonary nodules or occasionally cavities on chest imaging, such as metastatic lung cancer[21], sarcoidosis, silicosis, infectious diseases, LAM, pulmonary Langerhans cell histiocytosis, and Birt-Hogg-Dubé syndrome[22]. Research into typical PBML biomarkers for diagnosis is needed in the future.
For the treatment of PBML patients, there are three major approaches. Firstly, for asymptomatic PBML patients, long-term observation and follow-up with imaging examination without treatment can be chosen, as most PBML lesions are stable for long periods. Changes in hormones affect the development of BML lesions, thus, these lesions often shrink after the menopause and during pregnancy[23,24]. Therefore, antiestrogen therapy, including bilateral oophorectomy, gonadotropin-releasing hormone agonists, selective estrogen receptor modulators, and aromatase inhibitors, should be considered as second-line treatment options, especially for younger patients who have clinical manifestations[25]. Thirdly, for PBML patients with symptoms, especially symptoms secondary to the lesions (e.g., compression symptoms), who do not respond to antiestrogen therapy, surgical resection of PBML can be considered[26]. In one case report, a 36-year-old woman received seven procedures to remove 87 PBML lesions[27]; thus, mini-invasive local therapies, such as ablation, might be worthy of research.
Further characteristics of PBML patients are shown in Supplementary Tables 1 and 2.
In summary, the typical imaging manifestations of PBML are multiple nodules in the bilateral pulmonary fields, which are usually asymptomatic; uterine leiomyoma or a history of uterine leiomyoma; low or no metabolic activity on PET/CT; and extrauterine smooth-muscle cell proliferation on histopathology of biopsy samples. PBML can usually be diagnosed using these observations. Antiestrogen therapy and surgical resection should be considered for the treatment of PBML, which often has a good prognosis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chetty R, Ferrari F S-Editor: Liu M L-Editor: Webster JR E-Editor: Liu JH
| 1. | Steiner PE. Metastasizing fibroleiomyoma of the uterus: Report of a case and review of the literature. Am J Pathol. 1939;15:89-110.7. [PubMed] [Cited in This Article: ] |
| 2. | Itoh H, Yanagi M, Setoyama T, Shirao K, Yanagi S, Kataoka H, Shimotakahara T, Koono M. Solitary fibroleiomyomatous hamartoma of the lung in a patient without a pre-existing smooth-muscle tumor. Pathol Int. 2001;51:661-665. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Hull MT, Gonzalez-Crussi F, Grosfeld JL. Multiple pulmonary fibroleiomyomatous hamartomata in childhood. J Pediatr Surg. 1979;14:428-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Pacheco-Rodriguez G, Taveira-DaSilva AM, Moss J. Benign Metastasizing Leiomyoma. Clin Chest Med. 2016;37:589-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Patton KT, Cheng L, Papavero V, Blum MG, Yeldandi AV, Adley BP, Luan C, Diaz LK, Hui P, Yang XJ. Benign metastasizing leiomyoma: clonality, telomere length and clinicopathologic analysis. Mod Pathol. 2006;19:130-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 106] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Lee HJ, Choi J, Kim KR. Pulmonary benign metastasizing leiomyoma associated with intravenous leiomyomatosis of the uterus: clinical behavior and genomic changes supporting a transportation theory. Int J Gynecol Pathol. 2008;27:340-345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Abramson S, Gilkeson RC, Goldstein JD, Woodard PK, Eisenberg R, Abramson N. Benign metastasizing leiomyoma: clinical, imaging, and pathologic correlation. AJR Am J Roentgenol. 2001;176:1409-1413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Pitts S, Oberstein EM, Glassberg MK. Benign metastasizing leiomyoma and lymphangioleiomyomatosis: sex-specific diseases? Clin Chest Med. 2004;25:343-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Medarov BI, Khan MMHS, Modi A. Multiple Lung Masses in a Young Woman. JAMA. 2018;320:2141-2142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Xiao Z, Wang Y. [Benign metastasizing leiomyoma: A case report andliterature review]. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2019;44:951-956. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 11. | Taveira-DaSilva AM, Pacheco-Rodriguez G, Moss J. The natural history of lymphangioleiomyomatosis: markers of severity, rate of progression and prognosis. Lymphat Res Biol. 2010;8:9-19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Grafino M, Ferreira L, Telo L, Mira S, Alvoeiro M, Bárbara C. A rare cause of miliary pattern and respiratory failure - Benign metastasizing leiomyoma. Rev Port Pneumol (2006). 2016;22:296-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Tang EK, Wu FZ. Benign Metastasising Leiomyomatosis of the Lung Presenting as Progressive Pneumothorax. Heart Lung Circ. 2019;28:e94-e95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Hur JW, Lee S, Lee JB, Cho TH, Park JY. What are MRI findings of Spine Benign Metastasizing Leiomyoma? Case report with literature review. Eur Spine J. 2015;24 Suppl 4:S600-S605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Taveira-DaSilva AM, Alford CE, Levens ED, Kotz HL, Moss J. Favorable response to antigonadal therapy for a benign metastasizing leiomyoma. Obstet Gynecol. 2012;119:438-442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Miller J, Shoni M, Siegert C, Lebenthal A, Godleski J, McNamee C. Benign Metastasizing Leiomyomas to the Lungs: An Institutional Case Series and a Review of the Recent Literature. Ann Thorac Surg. 2016;101:253-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Orejola WC, Vaidya AP, Elmann EM. Benign metastasizing leiomyomatosis of the lungs presenting a miliary pattern. Ann Thorac Surg. 2014;98:e113-e114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Loukeri AA, Pantazopoulos IN, Tringidou R, Giampoudakis P, Valaskatzi A, Loukeri PA, Kampolis CF. Benign metastasizing leiomyoma presenting as cavitating lung nodules. Respir Care. 2014;59:e94-e97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Zhang J, Dong A, Cui Y, Wang Y, Chen J. Diffuse cavitary benign metastasising leiomyoma of the lung. Thorax. 2019;74:208-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Sawai Y, Shimizu T, Yamanaka Y, Niki M, Nomura S. Benign metastasizing leiomyoma and 18-FDG-PET/CT: A case report and literature review. Oncol Lett. 2017;14:3641-3646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Boitsios G, Bankier AA, Eisenberg RL. Diffuse pulmonary nodules. AJR Am J Roentgenol. 2010;194:W354-W366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Richards JC, Lynch DA, Chung JH. Cystic and nodular lung disease. Clin Chest Med. 2015;36:299-312, ix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Arai T, Yasuda Y, Takaya T, Shibayama M. Natural decrease of benign metastasizing leiomyoma. Chest. 2000;117:921-922. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Thomas EO, Gordon J, Smith-Thomas S, Cramer SF. Diffuse uterine leiomyomatosis with uterine rupture and benign metastatic lesions of the bone. Obstet Gynecol. 2007;109:528-530. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Lewis EI, Chason RJ, DeCherney AH, Armstrong A, Elkas J, Venkatesan AM. Novel hormone treatment of benign metastasizing leiomyoma: an analysis of five cases and literature review. Fertil Steril. 2013;99:2017-2024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 26. | Chen S, Zhang Y, Zhang J, Hu H, Cheng Y, Zhou J, Shen L, Chen H. Pulmonary benign metastasizing leiomyoma from uterine leiomyoma. World J Surg Oncol. 2013;11:163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Ottlakan A, Borda B, Lazar G, Tiszlavicz L, Furak J. Treatment decision based on the biological behavior of pulmonary benign metastasizing leiomyoma. J Thorac Dis. 2016;8:E672-E676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |