Abstract
Background
The purpose of this study was to identify clinicopathologic factors associated with positive peritoneal cytology (PPC) in patients with gastric cancer and to compare the overall survival (OS) of patients with PPC treated with and without neoadjuvant therapy.
Methods
The medical records of 3,747 patients with gastric or gastroesophageal adenocarcinoma presenting to our institution (January 1995 to December 2005) were reviewed to identify those patients who underwent diagnostic laparoscopy as a staging procedure prior to consideration for neoadjuvant therapy. Associations between various clinicopathologic factors and OS were examined with Cox proportional hazards models. Kaplan–Meier curves were created to compare OS between groups.
Results
Of 381 patients who underwent diagnostic laparoscopy for staging, 39 were found to have PPC without gross metastatic disease. Linitis plastica and tumors located at the gastroesophageal junction were identified as predictors of PPC (P < 0.01). Median follow-up for living patients was 51 months. Median OS for patients with PPC and no gross metastatic disease at laparoscopy (13 months) was no different from that for patients with gross metastatic disease at laparoscopy (10 months, P = 0.06). For the 39 patients with PPC and no gross metastatic disease, use of neoadjuvant therapy resulted in a 3-year OS rate of 12% versus 0% for patients who did not receive neoadjuvant therapy.
Conclusion
Outcomes for patients with PPC without gross metastatic disease are not significantly different from those patients with gross metastatic disease at laparoscopy. However, some patients can achieve long-term survival and should be considered for neoadjuvant treatment prior to attempts at surgical resection.
Similar content being viewed by others
The current National Comprehensive Cancer Network guidelines recommend considering laparoscopy in the workup of patients with potentially resectable gastric cancer.1 Given that peritoneal spread is common for patients with gastric cancer,2,3 the addition of peritoneal cytological analysis has been proposed to further increase accuracy in staging these patients.
The incidence of positive peritoneal cytology for patients with gastric cancer varies widely in the literature depending on the characteristics of the study population, with reported rates ranging from 4% to 41%.4–12 Clinical and pathologic factors that have been found to correlate with the presence of positive cytology are advanced disease stage, serosal tumor invasion, invasion of adjacent structures, age, lymphovascular invasion, and degree of tumor differentiation.4–9,11,12 The timing of peritoneal lavage also varies; some centers perform lavage at the time of laparotomy for resection while others perform lavage during diagnostic laparoscopy with plans for resection at a later date or following neoadjuvant treatment.
Positive cytology is well recognized as an indicator of both early recurrence and poor survival.4,11 The finding of free peritoneal cancer cells has even been suggested to represent stage IV incurable disease.10,13 Therefore the treatment recommendations for gastric cancer in the event of positive cytology range from palliative chemotherapy to attempts at neoadjuvant therapy followed by surgical resection. However, it is unclear if preoperative chemotherapy or chemoradiation can improve the dismal outcome associated with the finding of positive cytology. The purpose of this study was to compare the survival in patients treated with neoadjuvant therapy with that of patients treated without neoadjuvant therapy and consideration for surgery. In addition, we sought to identify clinicopathologic factors associated with the presence of positive cytology.
Methods
Patient Demographics and Clinicopathological Variables
The medical records of 3,747 patients with pathologically confirmed gastric or gastroesophageal adenocarcinoma presenting to The University of Texas M. D. Anderson Cancer Center from January 1, 1995 to December 31, 2005 were reviewed. We then selected those patients who underwent diagnostic laparoscopy as a staging procedure prior to consideration for neoadjuvant chemotherapy or chemoradiation. All patients were evaluated with computed tomography (CT) imaging of the abdomen, and most underwent evaluation with endoscopic ultrasonography. Patients were classified according to the 2002 American Joint Committee on Cancer (AJCC) staging criteria.14 The study was approved by the M. D. Anderson Institutional Review Board.
Clinical and pathologic data were retrospectively extracted from the medical records to include patient age and sex, tumor location (gastric, gastroesophageal junction, linitis plastica), pathologic stage, tumor histologic grade, and presence or absence of signet ring morphology. Exclusion criteria included distal esophageal cancer without involvement of the gastroesophageal junction, recurrent cancer, synchronous cancers, and palliative treatment. Findings from abdominal CT imaging were classified as either negative or equivocal for metastatic disease; patients with radiologically evident metastatic disease were excluded from the study. Findings from endoscopic ultrasonography were classified according to both T and N stage. Laparoscopic findings were categorized by the presence or absence of visible metastatic disease and positive or negative results on peritoneal cytological analysis. Neoadjuvant treatment included the administration of systemic chemotherapy with or without external-beam radiation therapy with the plan for curative resection. Treatment of patients with positive peritoneal cytology with neoadjuvant therapy was determined on an individual basis as the result of multidisciplinary discussions involving medical, surgical, and radiation oncology.
Surgical and Pathologic Technique
Diagnostic laparoscopy had been performed as a separate diagnostic procedure prior to the initiation of neoadjuvant chemoradiation therapy. A periumbilical Hasson port was placed so that the peritoneum and surfaces of the organs could be inspected. Ascites, if present, was aspirated and sent separate for cytological analysis. In the absence of obvious metastatic disease, 1 L of saline was infused into the peritoneal cavity and aspirated. Cytology specimens were concentrated by centrifugation. The resulting precipitate was placed on slides, smeared, and stained with the Papanicolaou technique using cytocentrifugation. Biopsy specimens from suspicious lesions were obtained and sent for permanent pathologic analysis. Each patient had a jejunostomy tube placed either laparoscopically or through an upper minilaparotomy incision, according to surgeon preference, to allow for adequate nutrition during the neoadjuvant therapy (as is our institutional policy).
Statistical Analysis
We tested for associations between various clinicopathologic factors and positive peritoneal cytology with the χ 2 test for categorical variables15 and the Wilcoxon rank sum test for continuous variables.16 Overall survival (OS) time was defined as the time from the date of diagnosis to date of death or last follow-up. We used the methodology proposed by Hosmer and Lemeshow for variable selection, whereby each covariate was tested independently in a Cox proportional hazards model (i.e., several univariable Cox proportional hazards models were constructed, yielding separate point and interval estimates for each variable). Upon completion of the univariable analyses, all variables significant at P ≤ 0.05 were included in the multivariable model, yielding a fully adjusted model.17,18 Three-year OS was estimated using the method of Kaplan and Meier.19,20 and the log-rank test was used to test for significant differences in OS.19,20 Computations were carried out using STATA software version 10 (StataCorp LP; College Station, TX). A P value of less than or equal to 0.05 was considered statistically significant.
Results
We identified 381 patients who underwent diagnostic laparoscopy as part of their evaluation for neoadjuvant therapy in the management of gastric and gastroesophageal adenocarcinoma. Median follow-up for living patients was 51 months. Two patients were lost to follow-up and excluded from the survival analysis. The clinicopathologic features of the study population are summarized in Table 1. Most patients had discrete gastric (43%) or gastroesophageal (45%) cancer with only a minority demonstrating linitis plastica (12%). The majority of patients (76%) had poorly differentiated tumors, and approximately half (48%) of the patients were noted to have signet ring morphology present in their cancer specimens.
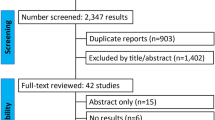
Computed tomography demonstrated equivocal evidence of metastatic disease in 33 (9%) patients. Endoscopic ultrasonography most commonly identified stage T3 primary tumors (71%) and N1 (51%) disease. On diagnostic laparoscopy, 83 patients (22%) were found to have visible metastatic disease which was confirmed on pathologic analysis. Of the 78% of patients without visible metastatic disease, cytologic analysis was performed in 262 patients and found to be positive for cancer cells in 39 (15%). A flowchart of the diagnostic and treatment pathways is presented in Fig. 1. Ultimately, the 39 patients with positive peritoneal cytology and no visible metastatic disease were managed with palliative treatment (N = 15) or neoadjuvant treatment (N = 24). Only 10 of the 24 patients treated with a neoadjuvant approach underwent surgery, of which 8 underwent resection and 2 patients were found to have unresectable disease.
Table 2 compares the clinical and pathologic characteristics of the patients with negative cytology and the patients with positive cytology without gross metastatic disease. The only factors associated with the finding of positive peritoneal cytology were tumor location at the gastroesophageal junction and the finding of linitis plastica.
Given the limited number of patients with positive peritoneal cytology, we performed separate Cox proportional hazards models for the clinicopathologic variables to identify significant individual associations with OS (Table 3). Linitis plastica (hazard ratio [HR] = 2.1, 95% confidence interval [CI] 1.46–3.03), suspicion of metastatic disease on CT imaging (HR = 1.81, 95% CI 1.21–2.72), gross metastases on laparoscopy (HR = 3.39, 95% CI 2.58–4.46), and positive peritoneal cytology (HR = 2.50, 95% CI 1.69–3.69) were noted to be associated with poorer OS. The ability to undergo surgical resection (HR = 0.18, 95% CI 0.13–0.23) was associated with a more favorable OS. When each of these variables was included in a fully adjusted multivariable model, the only significant factor associated with OS was the ability to undergo a surgical resection (HR = 0.24, 95% CI 0.17–0.35).
Overall survival in patients without gross metastatic disease at laparoscopy is demonstrated in Fig. 2, stratified by the presence or absence of positive cytology. As expected, the OS is significantly different between these two patient groups (P < 0.001). Overall survival in patients with positive cytology without gross metastatic disease and patients with gross metastatic disease at laparoscopy are depicted in Fig. 3. Median OS for patients with positive peritoneal cytology and no visible metastatic disease at laparoscopy was 12.8 months (95% CI 9.4–17.3) while median OS was 10.2 months (95% CI 7.6–11.6) for patients with gross metastatic disease at laparoscopy (P = 0.06). In an effort to identify the selection bias that could exist in selecting patients for either palliative or neoadjuvant treatment, we compared the clinical variables for these two groups in Table 4. Figure 4 shows the OS in patients with positive cytology without gross disease who received palliative treatment and were considered to have incurable stage IV disease versus patients treated with curative intent consisting of neoadjuvant therapy and the plan for potential resection. Median OS for patients treated with neoadjuvant therapy was 16.2 months (95% CI 10.8–26.5) compared with 7.2 months (95% CI 4.0–12.8) for patients treated with a palliative approach without consideration for neoadjuvant therapy and resection. For the patients with positive peritoneal cytology and no visible metastatic disease, use of neoadjuvant therapy resulted in a 3-year OS rate of 12% versus 0% for patients treated as having incurable stage IV disease (P = 0.005). There are three patients who had positive cytology and were treated with neoadjuvant therapy followed by resection who have demonstrated relatively long-term survival; these patients are alive at 28, 65, and 89 months.
Discussion
Fifteen percent of the patients without gross metastatic disease in our study were found to have positive peritoneal cytology. Predictors of the presence of positive cytology without visible metastatic disease are difficult to identify but included tumor location involving the gastroesophageal junction and the presence of linitis plastica. Our findings are notable for the many preoperative factors that were not predictive of positive cytology such as pathologic grade and endoscopic ultrasound stage. Positive cytology was a significant adverse prognostic indicator on univariable analyses but was not predictive of survival in a fully adjusted multivariable model. Of interest is that, in this retrospective evaluation of patients, curative intent treatment with neoadjuvant therapy was associated with improvement in median survival compared with patients treated with palliative intent. In addition, in the subset of patients in which surgical resection is achieved following neoadjuvant therapy there is the potential, although modest in frequency, for survival beyond 5 years.
The incidence of positive peritoneal cytology among studies similar to ours, and those which excluded patients with visible metastatic disease, ranges from approximately 4% to 8%.9–12 A study from Memorial Sloan–Kettering Cancer Center, which is similar to our study in both size and population demographics, reported an incidence rate of 6.5%.4 In general, the numbers of patients reported with positive peritoneal cytology have been small across all studies, with the largest published series consisting of 51 patients.11 The majority of the published studies evaluated their study population for predictors of positive cytology in an attempt to identify high-risk subsets of patients with gastric and gastroesophageal adenocarcinoma that should undergo cytological evaluation. Predictive factors identified included disease stage, serosal invasion, and tumor morphology.4,5,9,12 Our report evaluated only factors available preoperatively that could subsequently be used for patient selection for cytological assessment. Tumor location at the gastroesophageal junction and the finding of linitis plastica were associated with positive peritoneal cytology. Unfortunately, our results do not confirm the predictive value of other features that could be easily assessed preoperatively, such as tumor stage on endoscopic ultrasonography and pathologic characteristics of the tumor on initial biopsy.
Western reports of positive peritoneal cytology in patients with gastric cancer demonstrate uniformly poor survival, with median OS times of 4–15 months, and several centers describe 3-year survival rates of 0%.4–6,9,10 In contrast, reports from Asia describe a better outcome compared with Western studies with 5-year OS rates of 23–36%7,8 (with the exception of one center in Japan, which reported a 5-year OS rate of only 2%11). Controversy remains with respect to the association of positive peritoneal cytology and overall survival. In general, it has been reported that positive cytology is associated with poor overall survival4,11 while other reports, similar to ours, have not found positive cytology to be associated with overall survival when other clinical and pathologic factors were adjusted for in multivariable analysis.7
There are several limitations to our study. First, the number of patients identified with positive peritoneal cytology in the absence of gross metastatic disease is small (N = 39) and may have contributed to our inability to identify reliable predictors of positive cytology. Second, the generalizability of this finding is questionable outside of centers that perform diagnostic laparoscopy as a separate procedure prior to consideration of neoadjuvant therapy. However, other authors have recommended cytological analysis in patients with gastric cancer and agree with a neoadjuvant approach in patients found to have positive cytology.4,21 Third, the retrospective design and potential for selection bias may have contributed to the improved outcome in the patients selected for neoadjuvant therapy. We have attempted to address the potential for selection bias by listing clinical and preoperative variables for the two groups. This limitation is difficult to address as there is no universally accepted treatment approach to patients with positive cytology. One argument against a selection bias based on performance status or extent of disease is that all patients in this study were deemed potentially resectable prior to laparoscopy.
Future directions for research in this population at our institution should begin with the creation of a standard treatment protocol based on a multidisciplinary consensus between medical, radiation, and surgical oncologists. The potential for long-term survival demonstrated in this study would support attempting neoadjuvant treatment in all patients found to have positive cytology. The adverse prognostic implication of positive cytology is considerable, as demonstrated by the lack of a significant difference in OS between patients with visible metastatic disease and patients with positive cytology in the absence of visible disease. Without more effective systemic agents, it is unlikely that any approach will yield a major difference in OS. An interesting potential approach is the use of intraperitoneal chemotherapy, which some centers consider after neoadjuvant chemotherapy and resection in patients with positive cytology.4 The theoretical benefit to intraperitoneal chemotherapy is appealing in a population with only microscopic disease in the peritoneal cavity. A recent meta-analysis found improved OS in patients with advanced gastric cancer treated with hyperthermic intraoperative intraperitoneal chemotherapy, although consideration must be given to the increased morbidity.22 Regardless of the approach, multi-institutional collaboration would help resolve the questions surrounding the infrequent clinical scenario of isolated positive peritoneal cytology.
In summary, our current management strategy of performing diagnostic laparoscopy as a separate procedure prior to consideration of neoadjuvant therapy allows us to identify patients with positive peritoneal cytology without visible peritoneal disease. This finding is important in identifying a population that has traditionally been considered as having incurable disease. Based on our results, we conclude that some patients can achieve long-term survival and should be considered for neoadjuvant treatment prior to attempts at resection.
References
The Gastric Cancer Clinical Practice Guidelines in Oncology (Version 2.2007). ©2007 National Comprehensive Cancer Network, Inc. Available at: http://www.nccn.org. Accessed [2/29/08]
D’Angelica M, Gonen M, Brennan MF, et al. Patterns of initial recurrence in completely resected gastric adenocarcinoma. Ann Surg 2004;240:808–16
Maehara Y, Kakeji Y, Oda S, et al. Tumor growth patterns and biological characteristics of early gastric carcinoma. Oncology2001;61:102–12
Bentrem D, Wilton A, Mazumdar M, et al. The value of peritoneal cytology as a preoperative predictor in patients with gastric carcinoma undergoing a curative resection. Ann Surg Oncol2005;12:347–53
Ribeiro U Jr, Gama-Rodrigues JJ, Bitelman B, et al. Value of peritoneal lavage cytology during laparoscopic staging of patients with gastric carcinoma. Surg Laparosc Endosc1998;8:132–5
Ribeiro U Jr, Gama-Rodrigues JJ, Safatle-Ribeiro AV, et al. Prognostic significance of intraperitoneal free cancer cells obtained by laparoscopic peritoneal lavage in patients with gastric cancer. J Gastrointest Surg1998;2:244–9
Abe S, Yoshimura H, Tabara H, et al. Curative resection of gastric cancer: limitation of peritoneal lavage cytology in predicting the outcome. J Surg Oncol1995;59:226–9
Yoshikawa T, Tsuburaya A, Kobayashi O, et al. Peritoneal cytology in patients with gastric cancer exposed to the serosa–a proposed new classification based on the local and distant cytology. Hepatogastroenterology2003;50:1183–6
Bonenkamp JJ, Songun I, Hermans J, et al. Prognostic value of positive cytology findings from abdominal washings in patients with gastric cancer. Br J Surg1996;83:672–4
Burke EC, Karpeh MS Jr., Conlon KC, et al. Peritoneal lavage cytology in gastric cancer: an independent predictor of outcome. Ann Surg Oncol1998;5:411–5
Bando E, Yonemura Y, Takeshita Y, et al. Intraoperative lavage for cytological examination in 1,297 patients with gastric carcinoma. Am J Surg 1999;178:256–62
Suzuki T, Ochiai T, Hayashi H, et al. Peritoneal lavage cytology findings as prognostic factor for gastric cancer. Semin Surg Oncol1999;17:103–7
Japanese Gastric Cancer A. Japanese Classification of Gastric Carcinoma-2nd English Edition. Gastric Cancer1998;1:10–24
Greene FL, Page DL, Fleming ID, et al. AJCC Cancer Staging Manual, 6th edition. New York: Spring-Verlag, 2002
Fienberg S. The Analysis of Cross-Classified Categorical Data, 2nd edition. Cambridge: The MIT Press, 1983
Conover W. Practical Nonparametric Statistics, 2nd edition. New York: Wiley, 1980
Link C. Confidence intervals for the survival function using Cox’s proportional hazards model with covariates. Biometrics1984;40:601–10
Hosmer DW, Lemeshow S. Applied Survival Analysis, 1st edition. New York: Wiley, 1999
Fleming TH, Harrington DP. Nonparametric estimation of the survival distribution in censored data. Commun Stat1984; 4:2469–86
Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. New York: Wiley, 1980
Nakagawa S, Nashimoto A, Yabusaki H. Role of staging laparoscopy with peritoneal lavage cytology in the treatment of locally advanced gastric cancer. Gastric Cancer2007;10:29–34
Yan TD, Black D, Sugarbaker PH, et al. A systematic review and meta-analysis of the randomized controlled trials on adjuvant intraperitoneal chemotherapy for resectable gastric cancer. Ann Surg Oncol2007;14:2702–13
Acknowledgement
We would like to acknowledge Kristi M. Speights for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Badgwell, B., Cormier, J.N., Krishnan, S. et al. Does Neoadjuvant Treatment for Gastric Cancer Patients with Positive Peritoneal Cytology at Staging Laparoscopy Improve Survival?. Ann Surg Oncol 15, 2684–2691 (2008). https://doi.org/10.1245/s10434-008-0055-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-008-0055-3