Abstract
Asthma is an inflammatory disease and interleukin 12 (IL-12) may play a regulatory role in allergen-induced inflammation. The aim of this study was to investigate the association of polymorphisms in IL-12A/IL-12B with asthma. The asthma group included 198 adult patients and the control group included 453 individuals without asthma that were frequency-matched by gender and age. The distribution of genotypic and allelic frequencies of IL-12A rs568408 demonstrated significant differences between case and control groups. Specifically, the percentages of AA genotype of IL-12A rs568408 was significantly higher among asthmatic patients in Taiwan than healthy controls, compared to GG genotype. No significant difference was observed among the IL-12A rs2243115 and IL-12B rs3212227 genotypes between case and control groups. In addition, the A allele at IL-12A rs568408 was associated with more severe symptoms (P = 0.0085) among asthmatic patients. These results suggest that IL-12A rs568408 may contribute to the etiology and symptoms severity of asthma, indicating its usefulness as a predictive and diagnostic biomarker of asthma.
Similar content being viewed by others
Introduction
Asthma, the most common chronic respiratory disease, is a complex disorder that demonstrates variable phenotypes and an aberrant T helper 2 (Th2) cytokine profile1. Asthma is characterized by reversible airflow obstruction, airway inflammation, airway remodeling, and airway hyperresponsiveness2. Simplistically, asthma is divided into two subtypes: allergic and non-allergic3. Over the past 30 years, there has been a dramatic increase in the number of patients with asthma4, affecting >300 million people around the world5. Asthma involves the interaction of genetic and environmental components. The genetic contribution to asthma susceptibility was estimated to vary between 36% and 79%6, 7. The understanding that genomics play a role in the pathogenesis of asthma has been recognized for >100 years4. The exact mechanism of asthma pathogenesis, however, is still poorly understood. Asthma is characterized as a syndrome with various unidentifiable causes underlying its development and manifestation. It is difficult to identify specific causal genes and to determine if ethnic disparities should be attributed to the genetic contribution of this complex disorder. In recent years, >200 asthma candidate genes have been proposed by different approaches, including case-control association studies and positional cloning to investigate the phenotypic functions for the positive associated variants8, 9.
Cytokines play a pivotal role in regulation of the immune responses and the polymorphic nature of cytokine genes may confer flexibility of cellular immune phenomenum10. Recent evidence suggests that deficiency in the T helper 1/2 (Th1/Th2) cytokine pathway may underlie susceptibility to asthma11. IL-12 is an important immune-regulatory cytokine that demonstrates an antagonistic effect on the Th1/Th2 cytokine balance and provides a functional link between innate and acquired immune responses12. IL-12 is derived from dendritic cells, Langerhans cells, mononuclear phagocytic cells, and mast cells. IL-12 stimulates interferon production and activates and induces proliferation and cytokine production of natural killer cells13. Molecularly, IL-12 is a heterodimeric cytokine composed of two disulfide-linked polypeptide chains of molecular weights 35 (p35) and 40 (p40) kDa (encoded by IL-12A and IL-12B genes, respectively). IL-12 potently induces Th1 immune responses, while promoting maturation of cytotoxic T lymphocytes, stimulation of natural killer cells, and production of interferon-gamma (IFN-γ)14, 15. IL-12 also impairs neo-angiogenesis in tumor tissues through induction of IFN-γ-inducible protein-10 (IP-10)14. Because of these pleiotropic activities, IL-12 is regarded as one of the most feasible cytokines to be applied as immunotherapy for neoplasms16. Because IL-12 plays such as critical role in the immune response of intercellular and intracellular microenvironments, it is plausible that IL-12 genotypes may be determinants for individual susceptibility to human diseases, such as asthma. Previous studies have indicated that a single nucleotide polymorphism in the IL-12B gene (SNP; rs3212227) was significantly associated with a risk of a wide range of autoimmune and inflammatory diseases, such as psoriasis17, type-1 diabetes18, asthma-severity phenotype in Caucasians19, Crohn’s disease20, and rheumatoid arthritis21. Hirota and colleagues reported that the IL-12B rs3212227 polymorphism was significantly associated with a risk of childhood atopic asthma and was associated with high total immunoglobulin-E (IgE) levels in the Japanese population22. However, there are only limited studies to date that have examined the association between IL-12B genotypes and asthma risk, and the contribution of IL-12A genotypes to asthma is largely unknown. In 2011, Chen and colleagues reported that IL-12A rs568408 and IL-12B rs3212227 SNPs may individually and jointly contribute to asthma risk in a moderate population, 197 asthma patients and 369 controls in mainland China23. This is the first paper to examine the contribution of IL-12 genotypes to asthma susceptibility without any further analysis of clinical features or outcomes. The Taiwanese population has a similar genetic background (Han population) to mainland China, while more Western-style culture, different pollutant exposure and dietary habits of the island country. It is important to identify genomic biomarkers of asthma in the Taiwanese population, which has a high prevalence of more than 11% of asthmatic citizens. Therefore, in the current study, IL-12A rs568408, IL-12A rs2243115, and IL-12B rs3212227 polymorphisms were selected to investigate the associated risk of asthma in Taiwan, and their associations with clinical features, such as symptoms severity.
Results
The distributions of demographic and clinical characteristics of the investigated population are shown in Table 1. There was no statistical difference between the two groups with respect to age and gender (P = 0.2739 and 0.8999, respectively). However, differences in pulmonary functions, ratio of forced expiratory volume in the first second to forced vital capacity (FEV1/FVC, %) and percent of predicted FEV1 (FEV1%), were found between the case and control groups. The percentages of asthmatic patients with 1, 2, 3 and 4 stages of symptoms severity were 30.3, 32.8, 17.2 and 19.7%, respectively (Table 1).
Distribution of genotypic frequencies of the three investigated SNPs, rs568408 and rs2243115 in IL-12A and rs3212227 in IL-12B, are summarized in Table 2. The Hardy-Weinberg equilibrium (HWE) P-values of the controls at IL-12A rs568408, IL-12A rs2243115, and IL-12B rs3212227 are 0.2119, 0.0001 and 0.0009, respectively. The latter two SNPs deviated from HWE, probably due to small population sizes or presence of some inbreeding. Overall, there was a significant difference in the distribution of IL-12A rs568408 genotypes between cases and control groups (P = 0.0041), but not for those of IL-12A rs2243115 and IL-12B rs3212227 (both P > 0.05). Specifically, frequencies of the heterozygous variant AG and homozygous variant AA of IL-12A rs568408 were 24.7% and 7.6% in asthmatic cases and 21.6% and 2.5% in healthy controls, respectively. The AA genotype [odds ratio (OR) = 3.50, 95% confidence interval (CI) = 1.57–7.82, P = 0.0022], but not AG (OR = 1.28, 95% CI = 0.86–1.91, P = 0.2175), at IL-12A rs568408 demonstrated a statistically significant risk for asthma in Taiwan. The combined variant genotypes AG + AA did not further elevate asthma risk that the OR of AA alone (1.51 versus 3.50), compared to the wild-type GG genotype, indicating that A-allele of IL-12A rs568408 behaves as a recessive determinant to asthma risk. After adjusted with confounding factors for asthma, age and gender, the significance and trend still exist (Table 2).
The distribution of allelic frequencies of rs568408 and rs2243115 in IL-12A and rs3212227 in IL-12B are summarized in Table 3. As demonstrated in Table 3, the A allele at IL-12A rs568408 was associated with increased risk of asthma, compared to the G allele (OR = 1.63, 95% CI = 1.19–2.23, P = 0.0021). Specifically, the frequencies of the A and G alleles of IL-12A rs568408 were 19.9 and 80.1% in asthmatic patients and 13.2 and 86.8%, respectively, in controls (Table 3). By contrast, neither the G allele of IL-12A rs2243115 nor the C allele of IL-12B rs3212227 was associated with any significantly increased risk of asthma. The adjustments of confounding factors for asthma, age and gender, did not alter the significance and trend observed (Table 3).
Because age and gender may play a role in asthma, we were also interested in the interaction of the IL-12A rs568408 genotype with age and gender of the participants. In stratified analyses by age (Table 4), it appeared that the allelic frequencies of the A allele at IL-12A rs568408 was significantly higher in the asthma group than the control group among people of less than 37.7 years old (P = 0.0007), but not among people at the age ≥37.7 years old (P = 0.3876). As for gender analysis (Table 4), the A allele at IL-12A rs568408 was significantly higher in the asthma group than the control group among women (P = 0.0131), but not significant among men (P = 0.0593). The interaction of genotype-age and genotype-gender did not reach statistical significance (P for interaction = 0.09 and 0.72), likely due to small sample sizes.
We are interested in the association between IL-12A and IL-12B genotypes and asthma-relevant phenotypes. The distribution of allele frequencies of rs568408 and rs2243115 in IL-12A and rs3212227 in IL-12B and symptoms severity among asthmatic patients are shown in Table 5. From the data, it is found that the A allele frequencies at IL-12A rs568408 seemed to be lower than G allele frequencies among the patients in stage 1 and 2 (22.8 and 24.0% versus 32.2 and 35.0%, respectively), but higher than G allele frequencies among the patients in stage 3 and 4 (22.8 and 30.4% versus 15.8 and 17.0%, respectively), and the overall difference is statistically significant (P = 0.0085) (Table 5).
Discussion
In this hospital-based case-control study, we investigated the association of IL-12A rs568408, IL-12A rs2243115 and IL-12B rs3212227 polymorphisms and risk of asthma in Taiwan. The sample size is representative, containing 198 asthma patients and 453 age-matched and gender-matched healthy individuals (Table 1). We found that SNPs at IL-12A rs568408, but not IL-12A rs2243115 or IL-12B rs3212227 (Tables 2 and 3), were genomic determinants for asthma risk. In addition, the A allele at IL-12A rs568408 was associated with higher symptoms severity among asthmatic patients (Table 5). These findings support our hypothesis that functional polymorphisms in IL-12 may play a role in the initiation and progression of asthma.
In the literature, genotypic and phenotypic functions of IL-12B rs3212227 have been extensively studied and revealed. In 2001, it was reported by Morahan and colleagues that the IL-12B rs3212227 AA genotype was associated with significantly elevated expression of IL-12 among type 1 diabetes patients, with preferential transmission at this 3′-UTR polymorphism19. Soon after that in 2002, similar results were reported by Davoodi-Semiromi and colleagues using peripheral lymphocytes from type 1 diabetes patients in Caucasian-American families24. However, controversial results were reported by the following groups: In 2002, Seegers and colleagues reported that the presence of variant genotypes in IL-12B rs3212227 correlated with increased in vitro expression of IL-12A, but not IL-12B secretion25. In 2005, Yilmaz and colleagues found that individuals with the CC homozygous genotype at IL-12B rs3212227 had significantly higher IL-12 secretion levels from peripheral blood mononuclear cells stimulated by lipopolysaccharide and purified protein derivatives compared to those with AC heterozygous or AA homozygous genotypes26. As for cancer genomic studies, the CC/AC genotypes of IL-12B rs3212227 were associated with increased risk of esophageal cancer27, gastric cancer28, breast cancer29, bladder cancer30, cervical cancer31, 32, and osteosarcoma33, but some controversial findings were also found34,35,36,37. These inconsistencies may come from different use of inclusive and exclusive criteria during sample collection and different populations investigated. In addition, stimulation protocols and immunological status of patients were different. In our results, there was no association between the genotypes of IL-12B rs3212227 and asthma risk (Tables 2 and 3). Chen and colleagues reported that the AC genotype of IL-12B rs3212227 was associated with a borderline decreased risk of asthma compared with the AA genotype (P = 0.036)23. The subjects investigated were very similar between the Chen study and our study (controls versus cases = 369/197 versus 453/198). The percentage of AA, AC and CC genotypes was 36%, 49.1% and 14.9% in the Chen control population, and 35.8%, 41.5% and 22.7% in our control population.
In the current study, we identified a molecular risk biomarker, the AA genotype at IL-12A rs568408, for asthma susceptibility in early detection and prediction. This genotype was associated with elevated risk in several types of cancer, including esophageal cancer27, colorectal cancer37, liver cancer35, cervical cancer31, and osteosarcoma33. IL-12B can interact with IL-12A, in charge of formation of IL-12, IL-23A, and subsequent IL-23. Thus, the complicated and dynamic interaction among immune-proteins may play a very critical role in controlling immunoreactions in extracellular microenvironments. Thus, it is worthwhile for scientists to investigate the gene-gene interaction between IL-12A and IL-12B and their possibility to be novel determinants for asthma susceptibility, as is the case for cancer genomic etiology. In 2009, Chen and colleagues reported that IL-12A rs568408 GA/AA and IL-12B rs3212227 AC/CC variant genotypes were associated with a significantly increased risk of cervical cancer31. They proposed that the three SNPs in this study are located in conserved regions in mice, such that rs3212227 may disrupt exonic splicing silencers, and that rs568408 may disrupt exonic splicing enhancers and miRNAs binding31. Another novel finding in the current study was that the A allele at IL-12A rs568408 was associated with more severe symptoms among asthmatic patients (Table 5). However, the expression levels of IL-12 in investigated subjects were not available, which therefore limited our further analysis of the genotype-phenotype correlation and the possible association of phenotypic characteristics with prognosis and outcomes. In the near future, our findings could be validated in other asthma populations to determine if the AA IL-12A rs568408 genotype is a common genomic biomarker for asthma in these populations. Chen and his colleagues reported that the AG genotype of IL-12A rs568408 was associated with an increased risk of asthma compared to the GG genotype (P < 0.001)23, while they did not find any people with AA genotype and analyze the association of IL-12 genotypes with clinical features. Compared with their findings, the sample size of our study is of the same level (controls versus cases = 369/197 versus 453/198). In detail, percentages of GG, AG and AA genotypes was 80.2%, 19.8% and 0% in their control population, and 75.9%, 21.6% and 2.5% in ours. The lack of AA genotype at IL-12A rs568408 in the Chen population is unusual and was not observed in previous studies of other diseases performed in other areas of China31, 37, 38 or by the recording on National Center for Biotechnology Information website (https://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs = 3212227). The inconsistency may be related to differences in criteria of inclusion and exclusion during sample selection and collection.
There were some limitations in the current study. First, several asthma-related clinical information and phenotypes were not well recorded, such as the therapeutic responsiveness after bronchodilators and IgE levels. The restrictiveness limited us for further analysis about the role of IL-12 in asthma-related clinical outcomes. Second, the limited sample size may prone to lead false positive or negative findings due to lower statistical analyzing power. Third, the environmental factors such as occupational and allergen exposing status, which may serve as important confounding factors for asthma, were not well self-recalled and recorded.
Conclusion
The current study found that A allele at IL-12A rs568408 may act as a recessive determinant to asthma etiology and symptoms severity. We believe that our work may contribute to the understanding for the role of IL-12 in precise prediction, prevention and personalized strategies for asthma. Further investigations on the phenotypes of A allele at IL-12A rs568408 are needed.
Methods
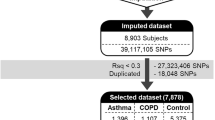
Study population
A total of 198 patients with asthma were recruited at China Medical University Hospital. The medical history was reviewed and recorded into the database. At the same time, 453 healthy individuals, who had been frequency-matched with asthma patients by gender and age (±5 years) and who had no previous history of asthma, were admitted to the same hospital for health screening (similar residential areas) and enrolled as matched controls. All individuals enrolled were provided with informed consent and the study was evaluated and approved by the Research Ethics Committee of China Medical University and Hospital (DMR100-IRB-284). All methods were performed in accordance with the relevant guidelines. The diagnosis and severity for each asthma patient were verified and agreed by at least two experienced pulmonary specialists according to the Global Initiative for Asthma (GINA) guidelines [The Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma (GINA) 2010. Available from: http://www.ginasthma.org]. Based on the clinical features presented, the patients were further categorized into four severity stages by the pulmonary specialists. The stage 1 is mild and stage 4 is severe. After the interview, 5 ml of venous blood was collected from each individual and used for DNA extraction and genotyping assays.
Genotyping conditions
Genomic DNA from peripheral blood leukocytes of patients and comparison individuals was prepared using the QIAamp Blood Mini Kit (Blossom, Taipei, Taiwan) and further processed as in our previous article39.
Primer sequences were designed as published by Chen and colleagues31. For IL-12A rs2243115 and rs568408, a mismatched A to replace C and a mismatched T to replace C were introduced into forward primers, respectively, at −3 bp from the polymorphic sites to create Bsen I and Nde I (New England BioLabs, Ipswich, MA, USA) digestible restriction sites. The primers were 5′-AGAAAAGACCTGTGAACAAAACGACT-3′ (forward) and 5′-AGATGGCTCACTAGATGCCAGG-3′ (reverse) for IL-12A rs2243115, and 5′-GAAGGATGGGACYATTACATCCATAT-3′ (forward) and 5′-CAGGATGGATATTTTCCCTTCT-3′ (reverse) for IL-12A rs568408. The variant allele IL-12A rs2243115G produced two fragments of 93 and 29 bp and the wild-type allele IL-12A rs2243115T generated one fragment of 122 bp. As for IL-12A rs568408, the wild-type allele IL-12A rs568408G produced 2 fragments of 98 and 23 bp and the variant allele IL-12A rs568408A resulted in one fragment of 121 bp. The primers of IL-12B rs3212227 were 5′-GATATCTTTGCTGTATTTGTATAGTT-3′ (forward) and 5′-AATATTTAAATAGCATGAAGGC-3′ (reverse), which generated a 118-bp fragment. Fragments were then digested by Taq I (New England BioLabs, Ipswich, MA, USA). The variant allele IL-12B rs3212227C produced 2 fragments of 92 and 26 bp, and the wild-type allele IL-12B rs3212227A resulted in a single 118-bp fragment.
Polymerase chain reaction (PCR) cycling conditions were performed as follows: one cycle at 94 °C for 5 min; 35 cycles of 94 °C for 30 s, 55 °C for 30 s, and 72 °C for 30 s; and a final extension at 72 °C for 10 min. Products were separated on a 3% agarose gel at 100 volts for 20 min. Genotype analysis was performed blinded by three independent researchers. Approximately 5% of the samples for each SNP were randomly selected for direct sequencing and the results from PCR-RFLP and direct sequencing were 100% concordant.
Statistical analyses
All of the 198 cases and 453 controls containing genotypic and clinical data were analyzed. To ensure that controls were representative of the general population and to exclude the possibility of genotyping error, the deviation of the genotype frequencies of IL-12 SNPs in the control subjects from those expected under the HWE was assessed using the goodness-of-fit test. Student’s t-test was used for comparison of average age and pulmonary functions between case and control group. Pearson’s chi-square test was used to compare the distribution of age group, gender, and IL-12 genotypes/SNP alleles between cases and controls. Logistic regression was used to estimate crude and adjusted ORs with 95% CIs. Any P < 0.05 was considered statistically significant.
References
Holgate, S. T. Genetics and environmental interactions in allergy and asthma. J Allergy Clin Immunol. 104, 1139–46 (1999).
Lai, T. et al. Interleukin-31 expression and relation to disease severity in human asthma. Sci Rep. 6, 22835 (2016).
Wardlaw, A. J. et al. New insights into the relationship between airway inflammation and asthma. Clin Sci. 103, 201–11 (2002).
Steinke, J. W., Rich, S. S. & Borish, L. Genetics of allergic disease. J Allergy Clin Immunol. 121, S384–7 (2008).
Himes, B. E. et al. Genome-wide association analysis identifies PDE4D as an asthma susceptibility gene. Am J Hum Genet 84, 581–93 (2009).
Koppelman, G. H. Gene by environment interaction in asthma. Curr Allergy Asthma Rep. 6, 103–11 (2006).
Barton, S. J. et al. PLAUR polymorphisms are associated with asthma, PLAUR levels, and lung function decline. J Allergy Clin Immunol. 123, 1391–400 (2009).
Ober, C. & Hoffjan, S. Asthma genetics 2006: the long and winding road to gene discovery. Genes Immun. 7, 95–100 (2006).
Zhang, J., Pare, P. D. & Sandford, A. J. Recent advances in asthma genetics. Respir Res. 9, 4 (2008).
Stanilova, S. & Miteva, L. Taq-I polymorphism in 3′UTR of the IL-12B and association with IL-12p40 production from human PBMC. Genes Immun. 6, 364–6 (2005).
Al-Daghri, N. M. et al. Th1/Th2 cytokine pattern in Arab children with severe asthma. Int J Clin Exp Med 7, 2286–91 (2014).
Miteva, L. & Stanilova, S. The combined effect of interleukin (IL)-10 and IL-12 polymorphisms on induced cytokine production. Hum Immunol. 69, 562–6 (2008).
Commins, S. P., Borish, L. & Steinke, J. W. Immunologic messenger molecules: cytokines, interferons, and chemokines. J Allergy Clin Immunol. 125, S53–72 (2010).
Del Vecchio, M. et al. Interleukin-12: biological properties and clinical application. Clin Cancer Res 13, 4677–85 (2007).
Emoto, Y. et al. Role of interleukin-12 in determining differential kinetics of invariant natural killer T cells in response to differential burden of Listeria monocytogenes. Microbes Infect. 10, 224–32 (2008).
Zabala, M. et al. Induction of immunosuppressive molecules and regulatory T cells counteracts the antitumor effect of interleukin-12-based gene therapy in a transgenic mouse model of liver cancer. J Hepatol. 47, 807–15 (2007).
Cargill, M. et al. A largescale genetic association study confirms IL12B and leads to the identification of IL23R as psoriasis-risk genes. Am J Hum Genet 80, 273–90 (2007).
Morahan, G. et al. Linkage disequilibrium of a type 1 diabetes susceptibility locus with a regulatory IL12B allele. Nat Genet. 27, 218–21 (2001).
Randolph, A. G. et al. The IL12B gene is associated with asthma. Am J Hum Genet 75, 709–15 (2004).
Zwiers, A. et al. Definition of polymorphisms and haplotypes in the interleukin-12B gene: association with IL-12 production but not with Crohn’s disease. Genes Immun. 5, 675–7 (2004).
Orozco, G. et al. Interleukin 12 (IL12B) and interleukin 12 receptor (IL12RB1) gene polymorphisms in rheumatoid arthritis. Hum Immunol. 66, 710–5 (2005).
Hirota, T. et al. Functional haplotypes of IL-12B are associated with childhood atopic asthma. J Allergy Clin Immunnol 116, 789–95 (2005).
Chen, T. et al. Association of single nucleotide polymorphisms in interleukin 12 (IL-12A and -B) with asthma in a Chinese population. Hum Immunol. 72, 603–6 (2011).
Davoodi-Semiromi, A., Yang, J. J. & She, J. X. IL-12p40 is associated with type 1 diabetes in Caucasian-American families. Diabetes. 51, 2334–6 (2002).
Seegers, D., Zwiers, A., Strober, W., Peña, A. S. & Bouma, G. A TaqI polymorphism in the 3′UTR of the IL-12 p40 gene correlates with increased IL-12 secretion. Genes Immun. 3, 419–23 (2002).
Yilmaz, V., Yentür, S. P. & Saruhan-Direskeneli, G. IL-12 and IL-10 polymorphisms and their effects on cytokine production. Cytokine. 30, 188–94 (2005).
Tao, Y. P. et al. Associations between polymorphisms in IL-12A, IL-12B, IL-12Rβ1, IL-27 gene and serum levels of IL-12p40, IL-27p28 with esophageal cancer. J Cancer Res Clin Oncol 138, 1891–900 (2012).
Yin, J. et al. Interleukin 12B rs3212227 T > G polymorphism was associated with an increased risk of gastric cardiac adenocarcinoma in a Chinese population. Dis Esophagus. 28, 291–8 (2015).
Kaarvatn, M. H. et al. Single nucleotide polymorphism in the interleukin 12B gene is associated with risk for breast cancer development. Scand J Immunol. 76, 329–35 (2012).
Ebadi, N. et al. Interleukin-12 and interleukin-6 gene polymorphisms and risk of bladder cancer in the Iranian population. Asian Pac J Cancer Prev. 15, 7869–73 (2014).
Chen, X. et al. Interactions of IL-12A and IL-12B polymorphisms on the risk of cervical cancer in Chinese women. Clin Cancer Res. 15, 400–5 (2009).
Roszak, A., Mostowska, A., Sowińska, A., Lianeri, M. & Jagodziński, P. P. Contribution of IL12A and IL12B polymorphisms to the risk of cervical cancer. Pathol Oncol Res. 18, 997–1002 (2012).
Wang, J. et al. Association of interleukin-12 polymorphisms and serum IL-12p40 levels with osteosarcoma risk. DNA Cell Biol. 32, 605–10 (2013).
Miteva, L., Stanilov, N., Deliysky, T., Mintchev, N. & Stanilova, S. Association of polymorphisms in regulatory regions of interleukin-12p40 gene and cytokine serum level with colorectal cancer. Cancer Invest. 27, 924–31 (2009).
Liu, L. et al. IL12 polymorphisms, HBV infection and risk of hepatocellular carcinoma in a high-risk Chinese population. Int J Cancer 128, 1692–6 (2011).
Huang, Z. Q., Wang, J. L., Pan, G. G. & Wei, Y. S. Association of single nucleotide polymorphisms in IL-12 and IL-27 genes with colorectal cancer risk. Clin Biochem. 45, 54–9 (2012).
Sun, R. et al. Interaction analysis of IL-12A and IL-12B polymorphisms with the risk of colorectal cancer. Tumour Biol. 36, 9295–301 (2015).
Li, L. J. et al. Interactions of interleukin-12A and interleukin-12B polymorphisms on the risk of intracranial aneurysm. Mol Biol Rep 39, 11217–23 (2012).
Hsia, T. C. et al. The contribution of interleukin-10 promoter genotypes to susceptibility to asthma in adults. In Vivo. 29, 695–9 (2015).
Acknowledgements
We appreciate Tissue-bank of China Medical University Hospital and Hsin-Ting Li and Shiou-Ting Yen for their excellent technical assistance. The consultants of statistical analysis from Chih-Hsin Muo and Cheng-Li Lin are very helpful in manuscript revision. This study is supported by China Medical University (CMU105-ASIA-17), China Medical University Hospital (DMR-106-022), and Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW106-TDU-B-212-113004).
Author information
Authors and Affiliations
Contributions
S.T., T.C., C.W., S.T., and B.D. carried out the conception and design, collection and assembly of data, dataanalysis and interpretation, and manuscript writing. W.S., C.C., H.C., and C.W. carried out the conception anddesign, collection and assembly of data, and data analysis and interpretation. All authors read and approved thefinal manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, TC., Tsai, CW., Chang, WS. et al. Association of Interleukin-12A rs568408 with Susceptibility to Asthma in Taiwan. Sci Rep 7, 3199 (2017). https://doi.org/10.1038/s41598-017-03523-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03523-0
This article is cited by
-
Genetic variants in miR-145 gene are associated with the risk of asthma in Taiwan
Scientific Reports (2022)
-
Genetic polymorphism in association with susceptibility to tuberculosis: a study in a Pakistani population
Brazilian Journal of Microbiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.