Abstract
Docetaxel in combination with prednisone is the standard of care in men with symptomatic castration-resistant prostate cancer (CRPC). However, a substantial proportion of men with CRPC do not benefit from docetaxel or other systemic therapy and those who do benefit invariably progress and die of (or with) prostate cancer. Resistance to chemotherapy in metastatic CRPC is a result of cellular mechanisms of drug resistance intrinsic to prostate cancer and general mechanisms common to different tumor types. Continued signaling from the androgen receptor, activation of oncogenic survival pathways by various receptor tyrosine kinases and crosstalk between the androgen receptor and these oncogenic survival pathways are hallmarks of progression of CRPC. General mechanisms of drug resistance include the existence of subpopulations of cancer cells with cellular mechanisms of resistance, resistance related to interactions between prostate cancer cells and their surrounding microenvironment and impaired drug delivery to the cancer cells. New therapeutics targeting these mechanisms are under evaluation in clinical trials. Drug resistance in metastatic CRPC is multifactorial and complex and development of new medical therapies remains challenging.
Key Points
-
Although the combination of docetaxel and prednisone prolongs survival and improves the quality of life of patients with metastatic castration-resistant prostate cancer (CRPC), the disease invariably progresses
-
Resistance to docetaxel and other types of systemic therapy can develop owing to mechanisms intrinsic to the biology of prostate cancer and/or general mechanisms of drug resistance common to different tumor types
-
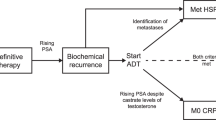
Cellular hallmarks of CRPC include continued signaling by the androgen receptor (AR), activation of various pathways associated with proliferation and survival, and crosstalk between the AR and these pathways
-
The existence of subpopulations of cancer cells with cellular mechanisms of resistance, interactions between cancer cells and their surrounding microenvironment, and impaired drug distribution can contribute to drug resistance in prostate cancer
-
New agents that target the critical cellular mechanisms of drug resistance are the most promising in metastatic CRPC; proof-of-principle clinical studies have shown activity for new agents targeting signaling from the AR and cellular mechanisms of resistance to taxanes
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Tredan, O., Galmarini, C. M., Patel, K. & Tannock, I. F. Drug resistance and the solid tumor microenvironment. J. Natl Cancer Inst. 99, 1441–1454 (2007).
Knight, Z. A., Lin, H. & Shokat, K. M. Targeting the cancer kinome through polypharmacology Nat. Rev. Cancer 10, 130–137 (2010).
Maximum androgen blockade in advanced prostate cancer: an overview of the randomised trials. Prostate Cancer Trialists' Collaborative Group. Lancet 355, 1491–1498 (2000).
Eisenberger, M. A. & Walsh, P. C. Early androgen deprivation for prostate cancer? N. Engl. J. Med. 341, 1837–1838 (1999).
Berthold, D. R. et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J. Clin. Oncol. 26, 242–245 (2008).
Tannock, I. F. et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N. Engl. J. Med. 351, 1502–1512 (2004).
Berthold, D. R., Pond, G. R., de Wit, R., Eisenberger, M. & Tannock, I. F. Survival and PSA response of patients in the TAX 327 study who crossed over to receive docetaxel after mitoxantrone or vice versa. Ann. Oncol. 19, 1749–1753 (2008).
Craft, N., Shostak, Y., Carey, M. & Sawyers, C. L. A mechanism for hormone-independent prostate cancer through modulation of androgen receptor signaling by the HER-2/neu tyrosine kinase. Nat. Med. 5, 280–285 (1999).
Zhu, M. L. & Kyprianou, N. Androgen receptor and growth factor signaling cross-talk in prostate cancer cells. Endocr. Relat. Cancer 15, 841–849 (2008).
Sharma, S. V. et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell 141, 69–80 (2010).
Feldman, B. J. & Feldman, D. The development of androgen-independent prostate cancer. Nat. Rev. Cancer 1, 34–45 (2001).
Gelmann, E. P. Molecular biology of the androgen receptor. J. Clin. Oncol. 20, 3001–3015 (2002).
Holzbeierlein, J. et al. Gene expression analysis of human prostate carcinoma during hormonal therapy identifies androgen-responsive genes and mechanisms of therapy resistance. Am. J. Pathol. 164, 217–227 (2004).
Shah, R. B. et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. Cancer Res. 64, 9209–9216 (2004).
Tomlins, S. A. et al. Integrative molecular concept modeling of prostate cancer progression. Nat. Genet. 39, 41–51 (2007).
Chen, C. D. et al. Molecular determinants of resistance to antiandrogen therapy. Nat. Med. 10, 33–39 (2004).
Tamura, K. et al. Molecular features of hormone-refractory prostate cancer cells by genome-wide gene expression profiles. Cancer Res. 67, 5117–5125 (2007).
Koivisto, P. et al. Androgen receptor gene amplification: a possible molecular mechanism for androgen deprivation therapy failure in prostate cancer. Cancer Res. 57, 314–319 (1997).
Stanbrough, M. et al. Increased expression of genes converting adrenal androgens to testosterone in androgen-independent prostate cancer. Cancer Res. 66, 2815–2825 (2006).
Montgomery, R. B. et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 68, 4447–4454 (2008).
Gregory, C. W., Johnson, R. T. Jr, Mohler, J. L., French, F. S. & Wilson, E. M. Androgen receptor stabilization in recurrent prostate cancer is associated with hypersensitivity to low androgen. Cancer Res. 61, 2892–2898 (2001).
Brooke, G. N. & Bevan, C. L. The role of androgen receptor mutations in prostate cancer progression. Curr. Genomics 10, 18–25 (2009).
Tremblay, A., Tremblay, G. B., Labrie, F. & Giguere, V. Ligand-independent recruitment of SRC-1 to estrogen receptor beta through phosphorylation of activation function AF-1. Mol. Cell. 3, 513–519 (1999).
Xu, J., Wu, R. C. & O'Malley, B. W. Normal and cancer-related functions of the p160 steroid receptor co-activator (SRC) family. Nat. Rev. Cancer 9, 615–630 (2009).
Wang, G., Wang, J. & Sadar, M. D. Crosstalk between the androgen receptor and beta-catenin in castrate-resistant prostate cancer. Cancer Res. 68, 9918–9927 (2008).
Wu, L., Birle, D. C. & Tannock, I. F. Effects of the mammalian target of rapamycin inhibitor CCI-779 used alone or with chemotherapy on human prostate cancer cells and xenografts. Cancer Res. 65, 2825–2831 (2005).
Boldt, S., Weidle, U. H. & Kolch, W. The role of MAPK pathways in the action of chemotherapeutic drugs. Carcinogenesis 23, 1831–1838 (2002).
Zelivianski, S. et al. ERK inhibitor PD98059 enhances docetaxel-induced apoptosis of androgen-independent human prostate cancer cells. Int. J. Cancer 107, 478–485 (2003).
Domingo-Domenech, J. et al. Interleukin 6, a nuclear factor-kappaB target, predicts resistance to docetaxel in hormone-independent prostate cancer and nuclear factor-kappaB inhibition by PS-1145 enhances docetaxel antitumor activity. Clin. Cancer Res. 12, 5578–5586 (2006).
Mimeault, M. et al. Combined targeting of epidermal growth factor receptor and hedgehog signaling by gefitinib and cyclopamine cooperatively improves the cytotoxic effects of docetaxel on metastatic prostate cancer cells. Mol. Cancer Ther. 6, 967–678 (2007).
Banerjee, S. et al. In vitro and in vivo molecular evidence for better therapeutic efficacy of ABT-627 and taxotere combination in prostate cancer. Cancer Res. 67, 3818–3826 (2007).
Lo Nigro, C. et al. The combination of docetaxel and the somatostatin analogue lanreotide on androgen-independent docetaxel-resistant prostate cancer: experimental data. BJU Int. 102, 622–627 (2008).
Raffo, A. J. et al. Overexpression of bcl-2 protects prostate cancer cells from apoptosis in vitro and confers resistance to androgen depletion in vivo. Cancer Res. 55, 4438–4445 (1995).
Zhang, M., Latham, D. E., Delaney, M. A. & Chakravarti, A. Survivin mediates resistance to antiandrogen therapy in prostate cancer. Oncogene 24, 2474–2482 (2005).
Yang, C. C. et al. Bcl-xL mediates a survival mechanism independent of the phosphoinositide 3-kinase/Akt pathway in prostate cancer cells. J. Biol. Chem. 278, 25872–25878 (2003).
Zoubeidi, A., Chi, K. & Gleave, M. Targeting the cytoprotective chaperone, clusterin, for treatment of advanced cancer. Clin. Cancer Res. 16, 1088–1093 (2010).
Yamanaka, K. et al. Induction of apoptosis and enhancement of chemosensitivity in human prostate cancer LNCaP cells using bispecific antisense oligonucleotide targeting Bcl-2 and Bcl-xL genes. BJU Int. 97, 1300–1308 (2006).
Pchejetski, D. et al. Chemosensitizing effects of sphingosine kinase-1 inhibition in prostate cancer cell and animal models. Mol. Cancer Ther. 7, 1836–1845 (2008).
Mumenthaler, S. M. et al. Pharmacologic inhibition of Pim kinases alters prostate cancer cell growth and resensitizes chemoresistant cells to taxanes. Mol. Cancer Ther. 8, 2882–2893 (2009).
Desgrosellier, J. S. & Cheresh, D. A. Integrins in cancer: biological implications and therapeutic opportunities. Nat. Rev. Cancer 10, 9–22 (2010).
Brown, J. M. & Wilson, W. R. Exploiting tumour hypoxia in cancer treatment. Nat. Rev. Cancer 4, 437–447 (2004).
Primeau, A. J., Rendon, A., Hedley, D., Lilge, L. & Tannock, I. F. The distribution of the anticancer drug doxorubicin in relation to blood vessels in solid tumors. Clin. Cancer Res. 11, 8782–8788 (2005).
Kyle, A. H., Huxham, L. A., Yeoman, D. M. & Minchinton, A. I. Limited tissue penetration of taxanes: a mechanism for resistance in solid tumors. Clin. Cancer Res. 13, 2804–2810 (2007).
Heldin, C. H., Rubin, K., Pietras, K. & Ostman, A. High interstitial fluid pressure—an obstacle in cancer therapy. Nat. Rev. Cancer 4, 806–813 (2004).
Semenza, G. L. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene 29, 625–634 (2010).
Kasper, S. Exploring the origins of the normal prostate and prostate cancer stem cell. Stem Cell Rev. 4, 193–201 (2008).
Maitland, N. J. & Collins, A. T. Prostate cancer stem cells: a new target for therapy. J. Clin. Oncol. 26, 2862–2870 (2008).
Visvader, J. E. & Lindeman, G. J. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat. Rev. Cancer 8, 755–768 (2008).
Komiya, A. et al. Neuroendocrine differentiation in the progression of prostate cancer. Int. J. Urol. 16, 37–44 (2009).
Meads, M. B., Gatenby, R. A. & Dalton, W. S. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat. Rev. Cancer 9, 665–674 (2009).
Kobayashi, H. et al. Acquired multicellular-mediated resistance to alkylating agents in cancer. Proc. Natl Acad. Sci. USA 90, 3294–3298 (1993).
Logothetis, C. J., Navone, N. M. & Lin, S. H. Understanding the biology of bone metastases: key to the effective treatment of prostate cancer. Clin. Cancer Res. 14, 1599–1602 (2008).
Logothetis, C. J. & Lin, S. H. Osteoblasts in prostate cancer metastasis to bone. Nat. Rev. Cancer 5, 21–28 (2005).
Zhang, J., Lu, Y. & Pienta, K. J. Multiple roles of chemokine (C-C Motif) ligand 2 in promoting prostate cancer growth. J. Natl Cancer Inst. 102, 522–528 (2010).
Qian, D. Z. et al. CCL2 is induced by chemotherapy and protects prostate cancer cells from docetaxel-induced cytotoxicity. Prostate 70, 433–442 (2010).
Fizazi, K. The role of Src in prostate cancer. Ann. Oncol. 18, 1765–1773 (2007).
Kavallaris, M. Microtubules and resistance to tubulin-binding agents. Nat. Rev. Cancer 10, 194–204 (2010).
Haldar, S., Basu, A. & Croce, C. M. Bcl2 is the guardian of microtubule integrity. Cancer Res. 57, 229–233 (1997).
Gottesman, M. M., Fojo, T. & Bates, S. E. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat. Rev. Cancer 2, 48–58 (2002).
Berrieman, H. K., Lind, M. J. & Cawkwell, L. Do beta-tubulin mutations have a role in resistance to chemotherapy? Lancet Oncol. 5, 158–164 (2004).
Seve, P. & Dumontet, C. Is class III beta-tubulin a predictive factor in patients receiving tubulin-binding agents? Lancet Oncol. 9, 168–175 (2008).
Verrills, N. M. et al. Alterations in gamma-actin and tubulin-targeted drug resistance in childhood leukemia. J. Natl Cancer Inst. 98, 1363–1374 (2006).
Bhalla, K. N. Microtubule-targeted anticancer agents and apoptosis. Oncogene 22, 9075–9086 (2003).
Attard, G. et al. Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, confirms that castration-resistant prostate cancer commonly remains hormone driven. J. Clin. Oncol. 26, 4563–4571 (2008).
Ryan, C. et al. Phase II multicenter study of chemotherapy (chemo)-naive castration-resistant prostate cancer (CRPC) not exposed to ketoconazole (keto), treated with abiraterone acetate (AA) plus prednisone [abstract]. J. Clin. Oncol. 27 (Suppl.), a5046 (2009).
Danila, D. C. et al. Phase II multicenter study of abiraterone acetate plus prednisone therapy in patients with docetaxel-treated castration-resistant prostate cancer. J. Clin. Oncol. 28, 1496–1501 (2010).
Tran, C. et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science 324, 787–790 (2009).
Scher, H. I. et al. Phase I-II study of MDV3100 in castration-resistant prostate cancer (CRPC) [abstract]. J. Clin. Oncol. 27, a151 (2009).
Attard, G., Cooper, C. S. & de Bono, J. S. Steroid hormone receptors in prostate cancer: a hard habit to break? Cancer Cell 16, 458–462 (2009).
Mendiratta, P. et al. Genomic strategy for targeting therapy in castration-resistant prostate cancer. J. Clin. Oncol. 27, 2022–2029 (2009).
Whang, J. E. et al. A phase II trial of lapatinib in hormone refractory prostate cancer [abstract]. J. Clin. Oncol. 26 (15S), a16037 (2008).
Gross, M. et al. A phase II trial of docetaxel and erlotinib as first-line therapy for elderly patients with androgen-independent prostate cancer. BMC Cancer 7, 142 (2007).
Gravis, G. et al. Results from a monocentric phase II trial of erlotinib in patients with metastatic prostate cancer. Ann. Oncol. 19, 1624–1628 (2008).
Canil, C. M. et al. Randomized phase II study of two doses of gefitinib in hormone-refractory prostate cancer: a trial of the National Cancer Institute of Canada-Clinical Trials Group. J. Clin. Oncol. 23, 455–460 (2005).
de Bono, J. S. et al. Open-label phase II study evaluating the efficacy and safety of two doses of pertuzumab in castrate chemotherapy-naive patients with hormone-refractory prostate cancer. J. Clin. Oncol. 25, 257–262 (2007).
De Bono, J. S. et al. Randomized phase II study of CNTO 328 (C), an anti-IL-6 monoclonal antibody, in combination with mitoxantrone (M) versus M alone in metastatic castration-resistant prostate cancer (CRPC) [abstract]. Genitourinary Cancer Symposium a86 (2010).
Sternberg, C. N. et al. Docetaxel plus oblimersen sodium (Bcl-2 antisense oligonucleotide): an EORTC multicenter, randomized phase II study in patients with castration-resistant prostate cancer. Ann. Oncol. 20, 1264–1269 (2009).
Saad, F. et al. A phase II randomized study of custirsen (OGX-011) combination therapy in patients with poor-risk hormone refractory prostate cancer who relapsed on or within six months of 1st-line docetaxel therapy [abstract]. J. Clin. Oncol. 26, a5002 (2008).
Jain, R. K. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307, 58–62 (2005).
Ning, Y. M. et al. Phase II trial of bevacizumab, thalidomide, docetaxel, and prednisone in patients with metastatic castration-resistant prostate cancer. J. Clin. Oncol. 28, 2070–2076 (2010).
Dahut, W. L. et al. Randomized phase II trial of docetaxel plus thalidomide in androgen-independent prostate cancer. J. Clin. Oncol. 22, 2532–2539 (2004).
Sonpavde, G. et al. Sunitinib malate for metastatic castration-resistant prostate cancer following docetaxel-based chemotherapy. Ann. Oncol. 21, 319–324 (2010).
Kelly, W. K. et al. A randomized double-blind placebo controlled phase III trial comparing docetaxel, prednisone and placebo with docetaxel, prednisone and bevacizumab in men with metastatic castration-resistant prostate cancer: survival results of CALGB 90401 [abstract]. J. Clin. Oncol. 28 (Suppl.), a4511 (2010).
Carducci, M. A. et al. A phase 3 randomized controlled trial of the efficacy and safety of atrasentan in men with metastatic hormone-refractory prostate cancer. Cancer 110, 1959–1966 (2007).
Tu, S. M. et al. Bone-targeted therapy for advanced androgen-independent carcinoma of the prostate: a randomised phase II trial. Lancet 357, 336–341 (2001).
Fizazi, K. et al. Phase II trial of consolidation docetaxel and samarium-153 in patients with bone metastases from castration-resistant prostate cancer. J. Clin. Oncol. 27, 2429–2435 (2009).
Nisson, S. et al. A randomized, placebo-controlled, phase 2 study of radium-223 in the treatment of metastatic hormone refractory prostate cancer (HRPC). Twelve months follow-up data [abstract]. Prostate Cancer Symposium a259, (2007).
Machiels, J. P. et al. Prospective randomized study comparing docetaxel, estramustine, and prednisone with docetaxel and prednisone in metastatic hormone-refractory prostate cancer. J. Clin. Oncol. 26, 5261–5268 (2008).
Garmey, E. G., Sartor, O., Halabi, S. & Vogelzang, N. J. Second-line chemotherapy for advanced hormone-refractory prostate cancer. Clin. Adv. Hematol. Oncol. 6, 118–122, 127–132 (2008).
Sternberg, C. N. et al. Multinational, double-blind, phase III study of prednisone and either satraplatin or placebo in patients with castrate-refractory prostate cancer progressing after prior chemotherapy: the SPARC trial. J. Clin. Oncol. 27, 5431–5438 (2009).
Sartor, A. O. et al. Cabazitaxel or mitoxantrone with prednisone in patients with metastatic castration-resistant prostate cancer (mCRPC) previously treated with docetaxel: final results of a multinational phase III trial (TROPIC) [abstract]. Genitourinary Cancer Symposium a9 (2010).
Lee, J. J. & Kelly, W. K. Epothilones: tubulin polymerization as a novel target for prostate cancer therapy. Nat. Clin. Pract. Oncol. 6, 85–92 (2009).
Acknowledgements
C. P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to researching the data for the article, discussions of the content, writing the article and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
I. F. Tannock has acted as a consultant for and received research support from Sanofi-Aventis. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Seruga, B., Ocana, A. & Tannock, I. Drug resistance in metastatic castration-resistant prostate cancer. Nat Rev Clin Oncol 8, 12–23 (2011). https://doi.org/10.1038/nrclinonc.2010.136
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2010.136
This article is cited by
-
Computer-aided analysis of quercetin mechanism of overcoming docetaxel resistance in docetaxel-resistant prostate cancer
Journal of Genetic Engineering and Biotechnology (2023)
-
Secreted miR-210-3p, miR-183-5p and miR-96-5p reduce sensitivity to docetaxel in prostate cancer cells
Cell Death Discovery (2023)
-
Combined in vitro/in vivo genome-wide CRISPR screens in triple negative breast cancer identify cancer stemness regulators in paclitaxel resistance
Oncogenesis (2023)
-
Bisphenol A contamination in processed food samples: an overview
International Journal of Environmental Science and Technology (2023)
-
Circ_0004087 interaction with SND1 promotes docetaxel resistance in prostate cancer by boosting the mitosis error correction mechanism
Journal of Experimental & Clinical Cancer Research (2022)