Abstract
Background
S-1 is an oral anticancer drug widely used in postoperative adjuvant therapy for patients in Japan with stage II/III gastric cancer. Candidates for more intense adjuvant treatments need to be identified, particularly among patients with stage III cancer.
Methods
Univariate and multivariate analyses were conducted for patients with stage II/III gastric cancer who underwent surgery and received S-1 postoperatively between 2000 and 2010.
Results
Factors indicating poor prognosis identified by univariate analysis include male sex (P = 0.022), age ≥67 years (P = 0.021), intestinal-type histology (P = 0.049), lymph node ratio ≥16.7 % (P < 0.0001), open surgery (P = 0.039), as well as the 13th JGCA stage (P < 0.0001) and the 14th JGCA/7th International Union Against Cancer (UICC) stage (P < 0.0001). Multivariate analysis revealed that lymph node ratio ≥16.7 % and intestinal-type histology were significant as predictors of prognosis, independent from the pathological stages. Based on these and other findings, stage IIIC cancer on the 14th JGCA/7th UICC stage system in combination with the lymph node ratio could identify patients with extremely high risk for recurrence
Conclusions
Our current findings suggest that lymph node ratio ≥16.7 % in combination with the new staging system could be a useful prognostic indicator in advanced gastric cancer. Because these high-risk patients cannot be identified preoperatively by any diagnostic tool, further improvement in postoperative adjuvant therapy is warranted.
Similar content being viewed by others
Introduction
Gastric cancer is the secondary leading cause of cancer death, so approximately 110,000 people in Japan would contract this disease each year, with 65,000 estimated deaths [1]. The mainstay of treatment is curative surgery [2]. However, many patients may have recurrence even after surgery. Therefore, various adjuvant chemotherapies have been developed to prevent recurrence after curative surgery [3–6]. S-1 is a fluoropyrimidine preparation combining tegafur, gimeracil, and oteracil potassium. The Adjuvant Chemotherapy Trial of S-1 for Gastric Cancer (ACTS-GC) was a randomized phase III trial in patients with the 13th Japan Gastric Cancer Association (JGCA) stage II/III gastric cancer [5, 7]. We participated in the trial and contributed to the establishment of the standard treatment in Japan [5].
The most commonly used staging system in gastric cancer is the TNM classification. This system was developed by the International Union Against Cancer (UICC) and has some similarities and differences from that used by the 13th JGCA edition. Recently, the 14th JGCA edition was published, which has become more consistent with the 7th edition of the UICC staging system [8–10]. It would be beneficial for both Eastern and Western gastroenterologists to interpret clinical outcomes using similar systems.
In the ACTS-GC trial, final outcomes [5-year relapse-free survival (RFS)] with the 13th JGCA stage II, IIIA, and IIIB cancer were 79.2, 61.4, and 37.6 % in the S-1 group and 64.4 %, 50.0 %, and 34.4 % in the surgery alone group, respectively [7]. An adjuvant effect of S-1 administration was robust, especially in subjects with stage II cancer. On the other hand, even with the use of S-1, clinical outcome among subjects with stage IIIA/IIIB disease was unsatisfactory. In the present study, we thus aimed to identify prognostic factors in the stage II/III gastric cancer patients who underwent curative surgery and postoperative administration of S-1 (standard treatment).
Materials and methods
Registration of patients
Between January 1, 2000 and December 31, 2010, 1,673 patients underwent gastrectomy for gastric adenocarcinoma in the gastrointestinal surgery division, Kitasato University Hospital. Among the 1,673 cases, 733 had advanced gastric cancer with depth of invasion beyond the muscularis propria. After exclusion of subjects with 13th JGCA stage IV disease (n = 191) and 13th JGCA stage IB disease (n = 146), a total of 396 patients with 13th JGCA stage II/III gastric cancer underwent gastrectomy with D1–D2 lymph node dissection, of which a further 67 patients who were given either neoadjuvant chemotherapy nor postoperative chemotherapy other than S-1 were excluded from the study. Of the remaining 329 patients, 172 who agreed to undergo adjuvant S-1 therapy and took S-1 for at least 1 day, form the basis of this study. The patients who showed poor compliance with S-1 were included. Of the study population, D1 lymph node dissection (n = 26) had been performed for the patients with a preoperative diagnosis of an early cancer (n = 12), those with severe comorbidities and elderly patients (n = 11), and for those with cancer of the gastric remnant who have already undergone D2 in the prior surgery (n = 3). These patients were not excluded.
The dose of S-1 was administered on the basis of body surface area: <1.25 m2 (80 mg daily); 0.1.25 m2 but <1.50 m2 (100 mg daily); and 0.1.50 m2 (120 mg daily). The adjuvant S-1 chemotherapy regimen was administered for 4 weeks followed by 2 weeks rest. This 6-week cycle was repeated principally during the first year after surgery. Toxicity of the chemotherapy was assessed on the basis of the Common Toxicity Criteria of the National Cancer Institute, version 4.0 (NCI-CTC) [11]. If patients had hematological toxic effects of grade 3 or 4 (highest possible grade) or nonhematological toxic effects of grade 2, 3 or 4, their daily dosage was reduced, or their treatment was postponed or stopped, according to each physician’s judgment.
JGCA and UICC classification differences
Several differences exist between the 13th and 14th JGCA classifications [8, 9]. In the 13th edition, the T category is classified into four categories. The descriptions are as follows: T1, the depth of invasion is mucosal or submucosal; T2, the depth of invasion is muscularis propria or subserosa; T3, the depth of invasion is serosa exposed; and T4, the depth of invasion is serosa infiltrating. On the other hand, in the 14th edition/7th UICC, the T category is classified into six categories. The descriptions are as follows: T1a, the depth of invasion is mucosal; T1b, the depth of invasion is submucosal; T2, the depth of invasion is muscularis propria; T3, the depth of invasion is subserosa; T4a, the depth of invasion is serosa exposed; and T4b, the depth of invasion is serosa infiltrating.
In the 13th edition, the status of lymph node metastasis is classified into four categories according to the anatomical classification of the involved lymph nodes. The descriptions are as follows: N0, no evidence of lymph node metastasis; N1, metastasis to the first tier of lymph nodes (restricted to perigastric lymph nodes), but no metastasis to the second and the third tier of lymph nodes (lymph nodes beyond perigastric lymph nodes; extraperigastric lymph nodes); N2, metastasis to the second tier of lymph nodes (extraperigastric regional lymph nodes), but no metastasis to the third tier of lymph nodes (lymph nodes beyond regional ones); and N3, metastasis to the third tier of lymph nodes. On the other hand, in the 14th edition, the status of lymph node metastasis is classified into four categories depending on the number of the involved lymph nodes. The descriptions are as follows: N0, there are no lymph nodes containing cancer cells; N1, there are cancer cells in 1–2 lymph nodes; N2, there are cancer cells in 3–6 lymph nodes; and N3, there are cancer cells in 7 or more lymph nodes (N3a, 7–15; N3b, 16 or more). In this study we used the 13th and 14th JGCA/7th UICC classifications, where the peritoneal cytology test must be included to define stage only in JGCA.
Clinicopathological factors
All histological and clinicopathological factors were assessed independently and blindly by histopathologists. Lymphatic permeation (ly) and vascular permeation (v) are defined as ly0, ly 1, ly 2, and ly 3 and v0, v1, v2, and v3 by infiltrative grade, but we classified ly and v as absence or presence. Percentage of metastatic lymph nodes, as lymph node ratio greater than or equal to a certain value designated by the researchers, has been defined as one of the most promising prognostic predictors by our previous studies [12–14] and elsewhere [15–18]. Histologically, there are two major types of gastric adenocarcinoma (Lauren’s classification). In this study, we classified cancers into diffuse type (por1, por2, sig, muc) and intestinal type (pap, tub1, tub2). Perioperative transfusion was also included as it has been reported to be a significant prognostic factor in advanced gastric cancer [19, 20]. It was defined as allogeneic blood transfusion during surgery or in the first 2 postoperative days.
Statistical analysis
Cumulative 5-year relapse-free survival (RFS) was estimated by the Kaplan–Meier method, and statistical difference was tested by the log-rank test. RFS was measured from the date of surgery to the date of recurrence or the last follow-up. Because the median duration of follow-up was only 26.5 months (range, 3–108 months), overall survival (OS) was not used in this study. Variables that had prognostic potential suggested by univariate analysis (P < 0.05) were subjected to multivariate analysis with the Cox proportional hazards regression model [21]. A value of P < 0.05 was considered statistically significant. All statistical analyses were done with SAS software package StatView, version 5.0 (SAS Institute, Cary, NC, USA) and/or JMP, version 5.0 (SAS Institute).
Results
Log-rank plot analysis
Among the 172 patients, 57, 79, and 36 had 13th JGCA stage II, IIIA, and IIIB cancer, respectively. We first made the log-rank plot analysis of lymph node ratio for RFS (Fig. 1). We calculated each P value and relative risk by the prognostic analysis by the log-rank method with a value of all 172 patients of lymph node ratio with log-rank plot [22]. The most suitable cutoff level was 16.7 %.
The most optimal cutoff values were defined according to the log-rank plot analysis of gastric cancer with pStage II/III who were treated by postoperative S-1 adjuvant therapy for recurrence-free survival (RFS). The most optimal cutoff values were 16.7 % according to P value (left panel) and relative risk (right panel). The most optimal cutoff values maximized relative risk as 4.8
Univariate and multivariate prognostic analysis
Clinicopathological features and prognosis in terms of RFS were analyzed in a univariate manner (Table 1. The seven variables for RFS that had prognostic potential in the univariate analysis (P < 0.05) were subjected to multivariate analysis. Results showed that lymph node ratio ≥16.7 and intestinal type of Lauren’s histology were prognostic factors independent of the 13th JGCA stage (Table 2), and those were also significant prognostic factors independent of the 14th JGCA/7th UICC stage (Table 3).
Lymph node ratio ≥16.7 as an independent prognostic factor
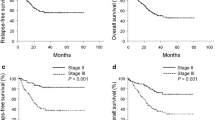
Lymph node ratio ≥16.7 was a significant prognostic factor for 13th JGCA stage II/III disease (P < 0.0001) (Fig. 2a). In the 13th JGCA Stage IIIA/IIIB subgroup, subjects with lymph node ratio ≥16.7 showed poorer prognosis than other cases, although differences did not reach statistical significance (P = 0.056 for stage IIIA and P = 0.088 for stage IIIB; Fig. 2c, d). Lymph node ratio ≥16.7 was not a significant prognostic factor for 14th JGCA/7th UICC stage IIIA/IIIB disease (Fig. 3b, c), although there was no case with lymph node ratio ≥16.7 in 14th JGCA/7th UICC stage II disease. Surprisingly, however, the lymph node ratio was relevant for prognostic stratification in patients with 14th JGCA/7th UICC stage IIIC disease (P = 0.0007) (Fig. 3d), and all 11 cases with lymph node ratio <16.7 are alive to date (median observed term, 30 months).
Prognostic analysis of lymph node ratio greater than or equal to 16.7 % for RFS by Kaplan–Meier estimates (according to 13th JGCA Stage). a Lymph node ratio ≥16.7 was significantly associated with poor outcome (P < 0.0001). b Lymph node ratio ≥16.7 was not associated with poor outcome in patients with 13th JGCA stage II disease. c Lymph node ratio ≥16.7 tended to be associated with poor outcome in patients with 13th JGCA stage IIIA disease (P = 0.056). d Lymph node ratio ≥16.7 tended to indicate poor outcome in patients with 13th JGCA stage IIIB disease (P = 0.088)
Prognostic analysis of lymph node ratio ≥16.7 for RFS, in the subgroup analysis of patients with 14th JGCA/7th UICC stage III disease. a Correlation diagram of lymph node ratio and the number of metastatic lymph nodes. b Lymph node ratio ≥16.7 was not associated with poor outcome in patients with 14th JGCA/7th UICC stage IIIA disease. c Lymph node ratio ≥16.7 was not associated with poor outcome with 14th JGCA/7th UICC stage IIIB. d Lymph node ratio ≥16.7 was relevant for prognostic stratification with 14th JGCA/7th UICC stage IIIC (P = 0.0007)
Separate analysis for clinical relevance of lymph node ratio ≥16.7 in D2 and D1 lymph node dissection
In the log-rank plot test restricted to only D2 dissection, the most optimal lymph node ratio was similar. The cutoff level most suitable for RFS was 18.4 % (see Online Resource Supplementary Fig. 1). The prognostic analysis of lymph node ratio only for D2 dissection cases (n = 146) turned out to be similar to that of total cases (n = 172) (see Online Resource Supplementary Figs. 2 and 3). The prognostic relevance of the lymph node ratio was also observed for the D1 population at the most optimal cutoff value of 17.5 %.
Enrichment of high-risk patients with recurrence using lymph node ratio and the 14th JGCA/7th UICC staging system
The lymph node ratio was determined to be an important prognostic factor independent of tumor stage, and a lymph node ratio ≥16.7 was a strong indicator of future recurrence. If we examine 5-year RFS of lymph node ratio ≥16.7 using 13th JGCA stage IIIB disease (n = 24) and 14th JGCA/7th UICC stage IIIC disease (n = 27), results are extremely dismal (36.7 and 28.2 %, respectively; Figs. 2d and 3d). There were 21 patients with lymph node ratio ≥16.7 with 13th JGCA stage IIIB disease who overlapped with 14th JGCA/7th UICC stage IIIC disease (Fig. 4a). There was no recurrence in the remaining 3 cases of lymph node ratio ≥16.7 with 13th JGCA stage IIIB disease, so we excluded these from the high-risk recurrence group (Fig. 4a, b). As a result, the 14th JGCA/7th UICC stage IIIC disease and lymph node ratio ≥16.7 added together identified a subset (n = 27) with extremely poor outcome, and a remarkable difference in survival was observed between this subset and the remainders of this study (n = 145; Fig. 4c).
Prognostic analysis identified a specific high-risk group of patients with 14th JGCA/7th UICC stage IIIC disease and lymph node ratio ≥16.7. a Relationship of 14th JGCA stage IIIC disease and 13th JGCA stage IIIB disease with lymph node ratio ≥16.7. The high-risk group was defined as composed of group 1 and group 2 (n = 27). b Group 1 and group 2 were associated with significantly worse outcome. The 5-year RFS was 33.3 % in group 1 and 27.2 % in group 2. c The high-risk group (group 1 + group 2) was associated with significantly worse outcome (P < 0.0001). The 5-year RFS was 81.7 % in the non-high-risk group and 28.2 % in the high-risk group
Discussion
In this study, we revealed the prognostic relevance of lymph node ratio among pStage II/III gastric cancer patients who underwent curative resection followed by postoperative administration of S-1. Lymph node ratio was identified as an independent prognostic factor according to the latest stage system (14th JGCA/7th UICC) (Table 2). RFS rather than OS was used at this time because median follow-up time remained insufficient at 26.5 months. Although there are several arguments regarding the adequacy of RFS as a surrogate endpoint, there is a trend to recognize this as a valid parameter in clinical trials evaluating postoperative adjuvant chemotherapy for gastric cancer because recurrence is almost consistent with disease progression and subsequent cancer death. Three-year RFS has actually been used as a primary endpoint in the recent Korean phase III trial exploring postoperative adjuvant treatment for gastric cancer [23]. Nevertheless, we would continue to validate our findings using OS in the future.
Primary aim of the current study was to identify a high-risk group for recurrence, and this is the first report showing that the lymph node ratio can identify patients who are at high risk for recurrence among those who underwent curative surgery followed by S-1 monotherapy. Lymph node ratio has already been reported as a prognostic factor in various series of advanced gastric cancer [12–18], but the prognostic relevance was observed again in this study with the Japanese population treated by the current standard of care.
In addition, we identified a specific group of high-risk patients with 14th JGCA/7th UICC stage IIIC disease and lymph node ratio ≥16.7 through a detailed prognostic analysis. Among these extremely high-risk patients (n = 27), 19 (70 %) have experienced recurrence, and 17 of 19 recurrences took place within 2 years after curative surgery. The lymph node ratio was supposed to be closely associated with the number of involved lymph nodes. We therefore anticipated that it may not be a relevant prognostic factor when used in combination with the 14th JGCA/7th UICC stage classification, which is based on the number of metastatic nodes. The lymph node ratio was significantly associated with the number of involved lymph nodes, as expected (Fig. 3a; R = 0.73; P < 0.0001), and its significance as a prognostic factor waned among 14th JGCA/7th UICC stage IIIA/IIIB disease (Fig. 3b, c). However, the lymph node ratio remained a potent prognostic factor for 14th JGCA/7th UICC stage IIIC disease (P = 0.0007) (Fig. 3d). The 11 cases with lymph node ratio <16.7 among the stage IIIC subgroup had an extremely large number of dissected lymph nodes (median, 61; range, 47–122), which possibly outnumbered the metastatic nodes (Table 4). For this population, the small lymph node ratio despite the large number of metastatic nodes might have reflected thoroughness of lymph node dissection, which compensated somewhat for the advanced disease status and resulted in favorable outcome. Had nodal dissection been less extensive, the lymph node ratio would have been higher and the prognosis correspondingly dismal. In this sense, lymph node ratio might be more sophisticated as a prognostic marker, reflecting quality of surgery as well as the biology of cancer.
On the other hand, there is an alternative explanation that the excellent outcome of patients with lymph node ratio <16.7 may reflect favorable immunological status. It is possible that a large number of negative lymph nodes can represent immune reactivity as a defensive mechanism to the metastasis of cancer cells. Even when a large number of lymph nodes harbored metastasis, existence of a larger number of nonmetastatic lymph nodes adjacent to these metastatic nodes may indicate that some anti-cancer process that favors the host is ongoing. In colon cancer, retrieval and examination of at least 12 lymph nodes has been established as an indicator of prognosis. As an explanation to this phenomenon, there is a hypothesis that patients who mount a stronger immune response to their cancers may have larger lymph nodes present in regional nodal basins, making them easier to find by pathologists [24].
To improve prognosis of aggressive gastric cancers such as type IV, large type III, or bulky N2 cases, intense regimens such as DCS (docetaxel/CDDP/S-1) are lately being explored in the neoadjuvant chemotherapy setting [25–27]. Perioperative chemotherapy has already been shown to be effective against aggressive gastric cancer in the Western world [4]. However, it is not currently possible to preoperatively identify patients with 14th JGCA/7th UICC pathological stage IIIC disease with lymph node ratio ≥16.7. Our data point to an urgent need for the development of a more intense and effective postoperative adjuvant chemotherapy, or establishment of a novel follow-up system (e.g., DNA detection) that allows for early detection of minimal tumor cells.
Conclusion
Our current findings suggest that lymph node ratio ≥16.7 could be useful as a prognostic indicator to identify high-risk patients with 14th JGCA/7th UICC stage IIIC gastric cancer. Establishment of intense postoperative therapeutic strategies for this target population is warranted.
References
Foundation for Promotion of Cancer Research. Cancer Statistics in Japan 2010. Available from http://ganjoho.ncc.go.jp/public/statistics/backnumber/2010_en.html. Accessed 30 June 2011.
Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Surgical treatment of advanced gastric cancer: Japanese perspective. Dig Surg. 2007;24:101–7.
Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–30.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36–46.
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29:4387–93.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 2nd English edition. Gastric Cancer. 1998;1:10–24.
Sobin LH, Wittekind CH, Gospodarowicz M (editors) International Union Againt Cancer (UICC): TNM classification of malignant tumors, 7th ed. New York: Wiley; 2009. p. 73–77.
Kikuchi S, Futawatari N, Sakuramoto S, Katada N, Yamashita K, Shibata T, et al. Comparison of staging between the old (6th edition) and new (7th edition) TNM classifications in advanced gastric cancer. Anticancer Res. 2011;31:2361–5.
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. Published: May 28, 2009.
Ooki A, Yamashita K, Kobayashi N, Katada N, Sakuramoto S, Kikuchi S, et al. Lymph node metastasis density and growth pattern as independent prognostic factors in advanced esophageal squamous cell carcinoma. World J Surg. 2007;31:2184–91.
Yamashita K, Sakuramoto S, Kikuchi S, Katada N, Kobayashi N, Watanabe M. Surgical resection of stage IV gastric cancer and prognosis. Anticancer Res. 2007;27:4381–6.
Yamashita K, Ooki A, Sakuramoto S, Kikuchi S, Katada N, Kobayashi N, et al. Lymph node metastasis density (ND)-factor association with malignant degree and ND40 as “non-curative factor” in gastric cancer. Anticancer Res. 2008;28:435–41.
Inoue K, Nakane Y, Iiyama H, Sato M, Kanbara T, Nakai K, et al. The superiority of ratio-based lymph node staging in gastric carcinoma. Ann Surg Oncol. 2002;9:27–34.
Nitti D, Marchet A, Olivieri M, Ambrosi A, Mencarelli R, Belluco C, et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol. 2003;10:1077–85.
Marchet A, Mocellin S, Ambrosi A, Morgagni P, Garcea D, Marrelli D, et al. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg. 2007;245:543–52.
Maduekwe UN, Lauwers GY, Fernandez-Del-Castillo C, Berger DL, Ferguson CM, Rattner DW, et al. New metastatic lymph node ratio system reduces stage migration in patients undergoing D1 lymphadenectomy for gastric adenocarcinoma. Ann Surg Oncol. 2010;17:1267–77.
Weitz J, D’Angelica M, Gonen M, Klimstra D, Coit DG, Brennan MF, et al. Interaction of splenectomy and perioperative blood transfusions on prognosis of patients with proximal gastric and gastroesophageal junction cancer. J Clin Oncol. 2003;21:4597–603.
Yamashita K, Sakuramoto S, Kikuchi S, Katada N, Kobayashi N, Watanabe M. Transfusion alert for patients with curable cancer. World J Surg. 2007;31:2315–22.
Cox DR. Regression models and life tables. J R Stat Soc. 1972;34:1987–2001.
Mandelker DL, Yamashita K, Tokumaru Y, Mimori K, Howard DL, Tanaka Y, et al. PGP9.5 promoter methylation is an independent prognostic factor for esophageal squamous cell carcinoma. Cancer Res. 2005;65:4963–8.
Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379:315–21.
Wong SL. Lymph node evaluation in colon cancer: assessing the link between quality indicators and quality. JAMA. 2011;306:1139–41.
Oyama K, Fushida S, Kinoshita J, Makino I, Nakamura K, Hayashi H, et al. Efficacy of pre-operative chemotherapy with docetaxel, cisplatin, and S-1 (DCS therapy) and curative resection for gastric cancer with pathologically positive para-aortic lymph nodes. J Surg Oncol. 2012;105:535–41.
Fushida S, Nashimoto A, Fukushima N, Kawachi Y, Fujimura T, Kuwabara S, et al. DCS Study Group. Phase II trial of preoperative chemotherapy with docetaxel, cisplatin and S-1 for T4 locally advanced gastric cancer. Jpn J Clin Oncol. 2012;42:131–3.
Katayama H, Ito S, Sano T, Takahari D, Mizusawa J, Boku N, Stomach Cancer Study Group of the Japan Clinical Oncology Group, et al. A Phase II study of systemic chemotherapy with docetaxel, cisplatin, and S-1 (DCS) followed by surgery in gastric cancer patients with extensive lymph node metastasis: Japan Clinical Oncology Group study JCOG1002. Jpn J Clin Oncol. 2012;42:556–9.
Acknowledgments
We thank the FORTE Science Communications, Tokyo, Japan, for editorial assistance.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1 The most optimal cutoff values were defined according to the log-rank plot analysis of gastric cancer with pStage II/III who were treated by postoperative S-1 adjuvant therapy after curative surgery with D2 dissection for RFS. The most optimal cutoff values were 18.4 % according to P value (left panel) and relative risk (right panel). The most optimal cutoff values maximized relative risk as 4.5.
Supplementary Fig. 2 Prognostic analysis of lymph node ratio greater than or equal to 18.4 % with D2 dissection for RFS by Kaplan–Meier estimates (according to the 13th JGCA stage). a Lymph node ratio ≥ 18.4 was significantly associated with poor outcome (P < 0.0001). b Lymph node ratio ≥ 18.4 was not associated with poor outcome in patients with 13th JGCA stage II disease. c Lymph node ratio ≥ 18.4 was not associated with poor outcome with 13th JGCA stage IIIA. d Lymph node ratio ≥ 18.4 was significantly associated with poor outcome with 13th JGCA stage IIIB (P = 0.041).
Supplementary Fig. 3 Prognostic analysis of lymph node ratio greater than or equal to 18.4 % with D2 dissection for RFS by Kaplan–Meier estimates (according to 14th JGCA/7th UICC Stage). a Lymph node ratio ≥ 18.4 was not associated with poor outcome in patients with 14th JGCA/7th UICC stage IIIA disease. b Lymph node ratio ≥ 18.4 was not associated with poor outcome with 14th JGCA/7th UICC stage IIIB. c Lymph node ratio ≥ 18.4 was relevant for prognostic stratification with 14th JGCA/7th UICC stage IIIC (P = 0.0002).
10120_2013_253_MOESM1_ESM.tif
Supplementary Fig. 1 The most optimal cut-off values were defined according to the log rank plot analysis of gastric cancer with pStage II/III who were treated by postoperative S-1 adjuvant therapy after curative surgery with D2 dissection for RFS. The most optimal cut-off values were 18.4% according to P value (left panel) and relative risk (right panel). The most optimal cut-off values maximized relative risk as 4.5(TIFF 77 kb)
10120_2013_253_MOESM2_ESM.tif
Supplementary Fig. 2 Prognostic analysis of lymph node ratio greater than or equal to 18.4% with D2 dissection for RFS by Kaplan-Meier estimates (according to the 13th JGCA Stage). a Lymph node ratio ≥18.4 was significantly associated with poor outcome (P<0.0001).b Lymph node ratio ≥18.4 was not associated with poor outcome in patients with the 13th JGCA stage II disease.c Lymph node ratio ≥18.4 was not associated with poor outcome with the 13th JGCA stage IIIA.d Lymph node ratio ≥18.4 was significantly associated with poor outcome with the 13th JGCA stage IIIB (P=0.041) (TIFF 101 kb)
10120_2013_253_MOESM3_ESM.tif
Supplementary Fig. 3 Prognostic analysis of lymph node ratio greater than or equal to 18.4% with D2 dissection for RFS by Kaplan-Meier estimates (according to the 14th JGCA/7th UICC Stage). a Lymph node ratio ≥18.4 was not associated with poor outcome in patients with the 14th JGCA/7th UICC stage IIIA disease.b Lymph node ratio ≥18.4 was not associated with poor outcome with the 14th JGCA/7th UICC stage IIIB.c Lymph node ratio ≥18.4 was relevant for prognostic stratification with the 14th JGCA/7th UICC stage IIIC (P=0.0002)(TIFF 88 kb)
Rights and permissions
About this article
Cite this article
Ema, A., Yamashita, K., Sakuramoto, S. et al. Lymph node ratio is a critical prognostic predictor in gastric cancer treated with S-1 chemotherapy. Gastric Cancer 17, 67–75 (2014). https://doi.org/10.1007/s10120-013-0253-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-013-0253-y