Abstract
Background
Chronic subdural haematoma (cSDH) is a frequent pathology in neurosurgery. Surgical treatment varies widely and is often characterised by repeated decompression. Therapeutic efficacy was evaluated by clinical symptom relief and haematoma reduction on preoperative and postoperative CT scans.
Methods
We investigated a consecutive series of 320 cases of cSDH between 2006 and 2010. In this series, the first- and second-line treatments were performed via hollow-screw placement under local anaesthesia, whereas enlarged burr holes under general anaesthesia were used as third-line treatment.
Results
In general, 63.3% of cases were sufficiently treated by a single operation, while 16.2% needed a second procedure with hollow screws. Only 20.5% needed open surgery by an enlarged burr hole with membranectomy under general anaesthesia. After the first operation, initial symptoms improved in 80.3% of cases, remained unchanged in 15.5% and worsened in 4.2% of cases. Mean age was 74.6 ± 12.1 years, with only one case of severe surgery-related complication.
Conclusions
Initial placement of hollow screws under local anaesthesia is a safe and sufficient treatment in most cases, and should be favoured as first-line treatment in patients with cSDH, since these patients are often of older age and present with distinct comorbidity.
Similar content being viewed by others
Introduction
The chronic subdural haematoma (cSDH) is a common pathology that occurs particularly among elderly patients. Its treatment is not standardised and varies widely, from craniotomy to enlarged burr holes, twist drill craniotomy with or without closed-system drainage and single-needle trephination [1, 5, 16, 21]. The cited series were performed without postoperative rinsing and showed a high incidence of early recurrence, causing repeated procedures.
As cSDH is often found in elderly and multimorbid patients, therapy for cSDH must reduce the patient’s stress as much as possible, but must also be effective in order to minimise the inpatient stay, which can produce secondary complications, such as pulmonary embolism, thrombosis and pneumonia.
To achieve sufficient drainage of the haematoma in as minimally invasive a manner as possible, and to prevent early and late recurrences, we used a simple bedside technique involving the placement of hollow screws [4]. In this series, the first- and second-line treatments were performed via hollow-screw placement under local anaesthesia, whereas enlarged burr holes under general anaesthesia were used as third-line treatment.
This study was designed to investigate the procedure’s therapeutic efficacy and safety. Therefore, we present this consecutive series of 320 cases, which were treated for symptomatic space-occupying cSDH with hollow-screw placement and closed-system drainage from 2006 and 2010 in our department.
Materials and methods
Patients
Hollow screws were placed with closed-system drainage for symptomatic space-occupying cSDH in 320 consecutive haematomas from 2006 and 2010 in our department.
Indication for primary surgery was if the haematoma exceeded the thickness of the skull or if a patient with a smaller haematoma was clinically symptomatic. Indications for revision surgery were symptomatic recurrence with no regard to haematoma size or asymptomatic haematoma recurrence exceeding the initial haematoma width.
There were 149 women (46.6%) and 171 men (53.4%), with a median age of 74.6 ± 12.1 years (range 25.0−97.7 years). Haematoma was located over the right hemisphere in 46.6% of cases, and over the left in 53.4%. Neurological symptoms that prompt cranial imaging and lead to a diagnosis of cSDH were classified using the Bender score [2]. The initial Bender score was 0 (no symptoms) in 2.5%, 1 (headache, seizures) in 58.1%, 2 in 37.1% (hemiparesis, drowsiness), and 3 (hemiplegia, unconsciousness) in 2.2% of cases. No case with a Bender score of 4 (comatose) was observed.
Imaging
CSDH was mainly diagnosed by computerised tomography (CT); rarely by magnetic resonance imaging (MRI). Follow-up was performed by CT scans. All patients with cSDH were included. However, cSDH with additional acute haemorrhage and hyperdense presentation on CT scan were also included as cSDH with additional subacute haemorrhage and isodense CT presentation did.
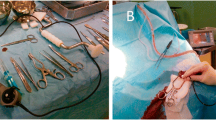
Hollow-screw placement
The hollow screw we used has an inner diameter of 3 mm and an outer diameter of 5 mm (Teleflex Medical, Belp, Switzerland) (Fig. 1). The screw is placed with a manual drill perpendicular to the skull under local anaesthesia, which is achieved using 5 ml of 2% mecain administered in the Trendelenburg position to avoid intracranial air as described earlier [4]. After placement, spontaneous cSDH outflow is usually observed and a three-way stopcock is connected afterwards to two syringes. Irrigation with warm Ringer’s solution is performed by alternating injection and suction until sufficient dilution of the haematoma. A collection bag is then connected as a closed system; the system is irrigated once daily and remains for 1–4 days, depending on its rate of outflow in the collection bag.
Postoperative evaluation
For every patient, neurological status was assessed before and after surgery. Neurological examination and CT scans were performed every 3 weeks postoperatively, until cSDH had completely dissolved on CT scans. In special cases, follow-up was individually adjusted.
Ethical standard
The study was conducted in accordance with the ethical standards of the Technical University of Munich, the local ethics committee (registration number: 4014/11) and the Declaration of Helsinki.
Statistical analysis
Chi-square or Fisher’s exact test was used. Differences between groups were tested by the Kruskall-Wallis test for non-parametric one-way analysis of variance (ANOVA), followed by Dunn’s test or the Student-Newman-Keuls test as post hoc tests. Differences between the two groups were tested with t-test or the Mann-Whitney-Wilcoxon test for multiple comparisons of ranks among independent samples. A p value of < 0.05 was considered significant. All results are presented as mean ± standard deviation (SD) (SigmaStat 3.5, Jandel Scientific, Erkrath, Germany).
Results
In general, 63.3% of cases were sufficiently treated by a single operation, while 16.2% needed a second operation with hollow screws. Only 20.5% needed open surgery under general anaesthesia by means of an enlarged burr hole with membranectomy (Fig. 2). Only one patient had to undergo standard craniotomy. On average, the first hollow screw was placed 44.4 ± 40.6 days after the supposedly responsible trauma. Mean drainage period was 1.8 ± 1.1 days and mean postoperative drainage volume was 128.9 ± 116.2 ml. In general, mean time until complete resolution of cSDH on follow-up examinations was 98.7 ± 82.8 days. During this time, a mean of 1.36 ± 0.6 procedures had to be performed, and mean inpatient stay was 10.4 ± 10.1 days. Mean age was 74.6 ± 12.1 years.
Causative event
In 54.7% of cases, head injury due to a fall or direct hit was the supposed origin, 5.9% occurred after intracranial surgery and 6.9% of cases had other causes, such as shunt placement or subarachnoid haemorrhage. In 32.5% of cases, no trauma was evident.
Symptom relief
Initial symptoms were within the reported wide range: headache in 31.6%, pseudodementia in 26.0%, paresis in 22.5%, dizziness in 17.2%, disturbed consciousness in 16.3% and epileptic seizures in 2.5% of cases. After the first hollow-screw placement, 80.3% of patients improved, 15.5% remained unchanged, and 4.2% showed clinical deterioration. After the second hollow-screw placement, 94.1% of patients improved clinically and 5.9% did not change, while no patient worsened clinically. After final burr-hole craniotomy, 95.0% of patients improved, 5.0% remained constant and none deteriorated clinically (Fig. 3). In terms of outcome, all patients were discharged without focal neurological deficit.
Influence of initial CT density on therapeutic course
In a preoperative CT scan, cSDH presented hypodense in 49.0%, isodense in 35.8% and hyperdense in 15.2% of cases. In these groups, mean width of cSDH ranged between 17.2 ± 7.0 and 17.8 ± 5.9 mm, while midline shift ranged between 6.0 ± 5.5 and 6.4 ± 4.3 mm without significant difference. Moreover, mean number of operations until complete regression was 1.40 ± 0.68 for hypodense, 1.33 ± 0.63 for isodense and 1.40 ± 0.50 for hyperdense cSDH (not significant).
Initial screw placement reduced the width of computertomographically hypodense cSDH by 27.9 ± 35.6%, isodense cSDH by 37.7 ± 20.2% and hyperdense cSDH by 33.7 ± 30.5% (not significant). Midline shift was reduced by 30.9 ± 51.1% for hypodense, 36.1 ± 34.7% for isodense and 45.1 ± 55.8% for hyperdense cSDH (not significant).
When cSDH presented hypodense on initial CT scan, a single operation was sufficient in 60.3% of cases, while a second screw placement was satisfactory in 18.1% of cases. Burr-hole placement with membranectomy under general anaesthesia was necessary in 21.6% of cases (Fig. 4a). For isodense-presenting cSDH, a single placement of hollow screws was sufficient in 62.3% of cases, whereas another screw placement was necessary in 19.7% of cases. However, general anaesthesia and burr-hole placement, including membranectomy, was still required in 18.0% of cases (Fig. 4a). Hyperdense-presenting subdural haematoma was sufficiently treated by a single operation in 75.5% of cases. However, a second screw placement was required in 7.5% of cases, and burr-hole placement with membranectomy and general anaesthesia was needed in 17.0% of cases (Fig. 4a).
Influence of initial septation
A preoperative CT scan showed septation in 34.8% and no septation in 65.2% of cases. Moreover, mean number of operations until complete regression was 1.69 ± 0.74 in septated cSDH and 1.24 ± 0.52 when septation was absent (p < 0.05). Primary placement of hollow screws reduced the width of septated cSDH by 17.7 ± 35.6%, and by 39.4 ± 23.7% when septation was absent (p < 0.05). Thus, midline shift was reduced by 20.2 ± 51.0% for septated cSDH and 43.7 ± 41.9% when septation was absent (p < 0.05). When cSDH was septated, 45.3% of cases were sufficiently treated by a single operation, compared with 77.0% when septation was absent (p < 0.05). A second operation with hollow screws was indicated in 19.8% when cSDH was septated and 11.8% when septation was absent. Thus, 34.9% of septated cSDH cases needed burr-hole placement with membranectomy under general anaesthesia, compared with 11.2% when there was no septation (Fig. 4b).
Anticoagulants and outcome
Anticoagulation was present in 57.2% of cases. Acetylsalicylic acid and coumarins were each consumed by 25.6% of patients. Clopidogrel was administered in 4.1%, and low-molecular heparin in 1.9% of cases. Anticoagulation was independent of placement site, density and septation. When anticoagulation was present, 1.35 ± 0.56 operations were needed for complete resolution of the cSDH, while 1.34 ± 0.52 operations were needed when anticoagulation was absent (not significant). Primary placement of hollow screws reduced the width of cSDH by 28.9 ± 33.2% when anticoagulation was present and midline shift was reduced by 32.6 ± 51.6%. In patients with no anticoagulation, haematoma was reduced by 37.8 ± 40.9% and midline shift was reduced by 37.9 ± 40.5% (not significant).
Perioperative complications
During inpatient stay, a wide range of perioperative complications arose. In terms of surgery-related incidents, we observed only one case requiring epidural haematoma evacuation, and five cases (1.6%) of postoperative meningitis. In general, 29.1% of all patients with cSDH experienced perioperative complications: bladder infection occurred in 16.6% of cases, seizures in 8.1% and pneumonia in 4.7%. Stroke occurred in 1.6% of patients, pulmonary embolism in 0.9% and thrombosis in 0.6%. Five patients (1.6%) died during their inpatient stay, for the above-mentioned reasons and as a result of severe comorbidity. No intraoperative deaths occurred.
Discussion
The presented study constitutes one of the largest published consecutive series of minimally invasive treatments for chronic subdural haematoma, and the largest series of treatment with hollow screws [4].
The epidemiological data for this series are similar to other published series concerning the treatment of cSDH, and the results are therefore comparable (Table 1) [1, 2, 12, 15, 18]. In this study, we subsumed cases of cSDH that were older than 3 weeks, as well as subacute subdural haematomas, which are defined as haematomas between 3 days and 3 weeks old.
The treatment of cSDH has two different goals. On the one hand, the space-occupying, continously expanding and potentially life-threatening haematoma has to be reduced. On the other hand, recurrence and surgery-related complications have to be avoided. Many different treatment options, such as craniotomy, burr-hole craniotomy, twist-drill craniotomy or needle trephination are able to decompress the haematoma [1, 18]. Thus, selecting the most suitable treatment must focus on reducing complications and minimising recurrence. It is well known that brain atrophy, causative trauma and coagulopathy begin a cycle of bleeding, hemostasis, fibrinolysis and rebleeding that leads to a progressive enlargement of the cSDH [7, 10, 12]. If this cycle is not stopped, haematoma persistence or recurrence is likely. As we are unable to influence the causal factors surgically, the applied surgical technique must permit sufficient haematoma evacuation, as well as thorough irrigation of the haematoma cavity, in order to remove the fibrinolytic substances [15].
The rate of incomplete haematoma evacuation in our series is within the reported range for treatment with open surgery burr-hole craniotomy or other minimally invasive techniques (Table 1; Figs. 2, 4a, b) [4, 14, 16, 17]. Moreover, many authors now state that complete operative removal of the cSDH is unnecessary as treatment, since drainage and irrigation are supposed to interrupt the pathophysiological cycle [3, 6, 12, 13]. Partial reduction of the cSDH, as documented by our data, sufficiently relieves the initial symptoms and modifies the imbalance of rebleeding and reabsorption towards reabsorption. This healing process might be initiated by improved local hyperfibrinolysis or reduced tensile forces on the macrocapillaries. Nevertheless, considerable volume reduction of the space-occupying haematoma is essential to initiate this process as also reported by others despite the lack of exact quantification of haematoma reduction in these studies [7, 8].
Moreover, we must be aware that in the presented series, hollow-screw placement was always used as a first-line treatment, even in patients with subacute haemorrhagic or highly septated cSDH (Figs. 2, 4a, b). Nevertheless, the rate of patients who finally had to undergo burr-hole craniotomy and membranectomy is low, compared with other series (Table 1) [1, 6, 13, 18, 20].
However, patients with a reduced chance of improvement via hollow screws may be identified by the appearance of a visibly-septated haematoma on the initial preoperative CT scan, as we showed septation to be a significant predictor for insufficient treatment by hollow screws in this series. This result can easily be explained. In cases with increasing septation, hollow screws are not able to reach all compartments of the cSDH, which is what causes insufficient decompression and irrigation of the cSDH. In such cases, open surgery with enlarged burr-hole trephination under general anaesthesia is required to perforate the membranes.
The fact that hyperdense haematoma requires fewer secondary hollow-screw placement procedures can be explained by two facts: on the one hand, hyperdense-presenting cSDH cases are acutely haemorrhagic, which causes a higher intracranial pressure (ICP) than cSDH without acute haemorrhage. Thus, a higher ICP might permit a more extensive initial evacuation of the haematoma. On the other hand, the more rapid deterioration of patients with hyperdense cSDH caused an increased tendency towards enlarged burr holes, once the primary hollow-screw placement had failed.
Mean inpatient stay was 10.4 ± 10.1 days and therefore also within the reported range of between 4.9 and 23 days of mean hospital stay [3, 6, 20].
Although perioperative non-surgical complications, such as bladder infection or seizures, were high, we observed fewer surgery-related complications than were reported after burr-hole craniotomy (Table 1) [17, 22]. Most importantly, we experienced no symptomatic intracerebral haemorrhage and no intraoperative deaths. Yet, overall mortality rate during inpatient stay was 1.6%, and therefore considerably low for treatment of usually multimorbid patients. Also, our reported surgery-related complication rate is very low compared with other studies (Table 1) [11, 15, 16]. Out of 320 cases, only one acute epidural haematoma occurred and five cases (1.6%) of postoperative meningitis were observed. This result is quite superior to most of the previous series, which report wound infection or meningitis in up to 18% of the patients, as reported by Smely et al. [20]. However, hollow-screw placement does not overcome the typical shortcomings and risks of conventional surgical therapy of cSDH, such as the risk of uncontrolled vascular damage with consecutive acute epidural, subdural or intracerebral bleeding requiring acute craniotomy and haematoma evacuation. Yet, in our series we only observed one case (0.3%) of epidural haematoma that required treatment. This rate is considerably higher in other series, which also reported procedure-related acute bleeding in between 2 and 3.3% of cases [17, 22].
Whether or not irrigation is crucial for successful treatment of cSDH, the literature is still conflicting. Even two recent randomised controlled trials were not able to answer this question sufficiently [9, 19].
However, this study also has several limitations. As a retrospective work, data can never be as reliable and complete as in a prospective set-up. Nonetheless, imaging data gathered was standardised and the conclusions drawn therefore seem to be of reliable strength, particularly when the large number of enrolled patients is considered.
Another application of the hollow screw used is the diagnostic puncture for presumed epidural or subdural empyema. In cases when the patient’s history, CT findings and MRI findings are unclear with regard to the differential diagnosis regarding epidural or subdural haematoma and empyema, diagnostic puncture under local anaesthesia is an option to avoid potentially unnecessary general anaesthesia. As the inner diameter of 3 mm is considerably larger than needle trephination, hollow screws are highly applicable for diagnostic sampling, even of viscous pus.
Conclusions
Primary treatment of cSDH by hollow screws under local anaesthesia is a safe, sufficient, and well-tolerated therapy in most cases. It has a high rate of initial success, especially in patients with non-septated haematomas. Therefore, it should be favoured as a first-line method of treatment in cSDH cases, keeping in mind that most of these patients are elderly and experience multiple comorbidity. In conclusion, 79.5% of these patients were sufficiently treated by hollow screws, with a low rate of procedure-related complications.
References
Aoki N (1984) Subdural tapping and irrigation for the treatment of chronic subdural hematoma in adults. Neurosurgery 14:545–548
Bender MB, Christoff N (1974) Nonsurgical treatment of subdural hematomas. Arch Neurol 31:73–79
Camel M, Grubb RL Jr (1986) Treatment of chronic subdural hematoma by twist-drill craniotomy with continuous catheter drainage. J Neurosurg 65:183–187
Emonds N, Hassler WE (1999) New device to treat chronic subdural hematoma–hollow screw. Neurol Res 21:77–78
Ernestus RI, Beldzinski P, Lanfermann H, Klug N (1997) Chronic subdural hematoma: surgical treatment and outcome in 104 patients. Surg Neurol 48:220–225
Gilsbach J, Eggert HR, Harders A (1980) [External closed drainage treatment of chronic subdural hematomas after bore-hole trepanation]. Unfallchirurgie 6:183–186
Ito H, Saito K, Yamamoto S, Hasegawa T (1988) Tissue-type plasminogen activator in the chronic subdural hematoma. Surg Neurol 30:175–179
Ito H, Yamamoto S, Saito K, Ikeda K, Hisada K (1987) Quantitative estimation of hemorrhage in chronic subdural hematoma using the 51Cr erythrocyte labeling method. J Neurosurg 66:862–864
Javadi A, Amirjamshidi A, Aran S, Hosseini SH (2011) A randomized controlled trial comparing the outcome of burr-hole irrigation with and without drainage in the treatment of chronic subdural hematoma: a preliminary report. World Neurosurg 75:731–736, discussion 620-733
Kawakami Y, Chikama M, Tamiya T, Shimamura Y (1989) Coagulation and fibrinolysis in chronic subdural hematoma. Neurosurgery 25:25–29
Kotwica Z, Brzezinski J (1991) Chronic subdural haematoma treated by burr holes and closed system drainage: personal experience in 131 patients. Br J Neurosurg 5:461–465
Markwalder TM (1981) Chronic subdural hematomas: a review. J Neurosurg 54:637–645
Markwalder TM, Steinsiepe KF, Rohner M, Reichenbach W, Markwalder H (1981) The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg 55:390–396
Okada Y, Akai T, Okamoto K, Iida T, Takata H, Iizuka H (2002) A comparative study of the treatment of chronic subdural hematoma—burr hole drainage versus burr hole irrigation. Surg Neurol 57:405–409, discussion 410
Ram Z, Hadani M, Sahar A, Spiegelmann R (1993) Continuous irrigation-drainage of the subdural space for the treatment of chronic subdural haematoma. A prospective clinical trial. Acta Neurochir (Wien) 120:40–43
Reinges MH, Hasselberg I, Rohde V, Kuker W, Gilsbach JM (2000) Prospective analysis of bedside percutaneous subdural tapping for the treatment of chronic subdural haematoma in adults. J Neurol Neurosurg Psychiatry 69:40–47
Rohde V, Graf G, Hassler W (2002) Complications of burr-hole craniostomy and closed-system drainage for chronic subdural hematomas: a retrospective analysis of 376 patients. Neurosurg Rev 25:89–94
Sambasivan M (1997) An overview of chronic subdural hematoma: experience with 2300 cases. Surg Neurol 47:418–422
Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, Richards HK, Marcus H, Parker RA, Price SJ, Kirollos RW, Pickard JD, Hutchinson PJ (2009) Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet 374:1067–1073
Smely C, Madlinger A, Scheremet R (1997) Chronic subdural haematoma--a comparison of two different treatment modalities. Acta Neurochir (Wien) 139:818–825
Tabaddor K, Shulmon K (1977) Definitive treatment of chronic subdural hematoma by twist-drill craniostomy and closed-system drainage. J Neurosurg 46:220–226
van Eck AT, de Langen CJ, Borm W (2002) Treatment of chronic subdural haematoma with percutaneous needle trephination and open system drainage with repeated saline rinsing. J Clin Neurosci 9:573–576
Acknowledgements
This study was completely financed by institutional grants from the Department of Neurosurgery.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
This paper presents the results of a retrospective analysis of a quite large series of chronic subdural haematomas treated by hollow-screw drainage. It is an interesting study, although retrospective, and therefore with the drawbacks associated with such a design. The analysis focuses on recurrence rate and explores the influence of factors such as initial CT density, presence of septations and coagulation state on the therapeutic course and outcome.
CSDH, as the authors note, is a common entity in neurosurgical practice. It deserves to be noted, and awareness of recurrences and problems in the treatment of cSDH is important. As such, this manuscript is welcomed.
Domenico d’Avella
Padova, Italy
Rights and permissions
About this article
Cite this article
Krieg, S.M., Aldinger, F., Stoffel, M. et al. Minimally invasive decompression of chronic subdural haematomas using hollow screws: efficacy and safety in a consecutive series of 320 cases. Acta Neurochir 154, 699–705 (2012). https://doi.org/10.1007/s00701-012-1294-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1294-4