Abstract
Purpose
Integration of high-risk human papillomavirus (HR-HPVs) into the host DNA has been proposed as a risk for cervical carcinogenesis. HPV-16 is the predominant high-risk type and its integration ration varied largely in different cervical cancer (CC) samples. The aim of this study was to evaluate the correlation between physical state of HPV16 infection and extent of cervical lesion, as well as the clinical significance of virus existing state.
Methods
A total of 252 cases of paraffin-embedded blocks derived from cancer precursor lesion and cervical carcinoma samples were detected by HC-II for HR-HPV infection. HPV16 infection was confirmed by PCR and immunohistochemistry for HPV16 E7 simultaneously. The physical state of HPV16 infection were assessed by PCR for 3 overlapping fragments in E2 gene and multiple PCR for E2 gene and E7 gene.
Results
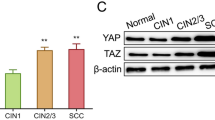
The infection ratio of HR-HPV in normal cervical tissue, cervical intraepithelial neoplasia (CIN) I, CIN II, CIN III and cervical cancer were 15.0, 32.8, 54.3, 69.7, 93.8%, respectively. HR-HPV positive samples of 62.8% were infected with HPV16. The integration ratio of HPV16 in CIN III and cervical carcinoma were 35.7 and 58.1% respectively, both of which were significantly higher than that of CIN I and normal cervical tissues. The discrepancy was statistically significant (P < 0.05). Furthermore, it was observed that persistent virus infection and progression of cervical lesion were more common in CIN I with integrated HPV16 than that with episomal HPV16.
Conclusion
The integration ratio of HPV16 was accompanied by an increase in the grade of cervical lesion. The integrated state of HPV16 infection was strongly associated with persistent HPV infection and progression of cervical lesions.


Similar content being viewed by others
Change history
10 March 2020
The authors would like to correct figure, as the error was introduced in the preparation of this figure for publication. We sincerely apologize for having this error in the article, the authors have provided corrected version of figure here.
10 March 2020
The authors would like to correct figure, as the error was introduced in the preparation of this figure for publication. We sincerely apologize for having this error in the article, the authors have provided corrected version of figure here.
Abbreviations
- CC:
-
Cervical cancer
- HR-HPVs:
-
High-risk human papillomavirus
- CIN:
-
Cervical intraepithelial neoplasia
References
Arends MJ, Buckley CH, Wells M (1998) Aetiology, pathogenesis, and pathology of cervical neoplasia. J Clin Pathol 51:96–103
Badaracco G, Venuti A, Sedati A, Marcante ML (2002) HPV16 and HPV18 in genital tumors: significantly different levels of viral integration and correlation to tumor invasiveness. J Med Virol 67:574–582
Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R, Shah KV (1995) Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst 87:796–802
Castle PE, Wheeler CM, Solomon D, Schiffman M, Peyton CL (2004) Interlaboratory reliability of Hybrid Capture 2. Am J Clin Pathol 122:238–245
Gallo G, Bibbo M, Bagella L, Zamparelli A, Sanseverino F, Giovagnoli MR, Vecchione A, Giordano A (2003) Study of viral integration of HPV–16 in young patients with LSIL. J Clin Pathol 56:532–536
Graham DA, Herrington CS (2000) HPV-16 E2 gene disruption and sequence variation in CIN 3 lesions and invasive squamous cell carcinomas of the cervix: relation to numerical chromosome abnormalities. Mol Pathol 53:201–206
Ishiji T (2000) Molecular mechanism of carcinogenesis by human papillomavirus-16. J Dermatol 27:73–86
Jeon S, Lambert PF (1995) Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: implications for cervical carcinogenesis. Proc Natl Acad Sci USA 92:1654–1658
Jeon S, Allen-Hoffmann BL, Lambert PF (1995) Integration of human papillomavirus type 16 into the human genome correlates with a selective growth advantage of cells. J Virol 69:2989–2997
Kalantari M, Blennow E, Hagmar B, Johansson B (2001) Physical state of HPV16 and chromosomal mapping of the integrated form in cervical carcinomas. Diagn Mol Pathol 10:46–54
Klaes R, Woerner SM, Ridder R, Wentzensen N, Duerst M, Schneider A, Lotz B, Melsheimer P, von Knebel Doeberitz M (1999) Detection of high-risk cervical intraepithelial neoplasia and cervical cancer by amplification of transcripts derived from integrated papillomavirus oncogenes. Cancer Res 59:6132–6136
Kulmala SM, Syrjänen SM, Gyllensten UB, Shabalova IP, Petrovichev N, Tosi P, Syrjänen KJ, Johansson BC (2006) Early integration of high copy HPV16 detectable in women with normal and low grade cervical cytology and histology. J Clin Pathol 59(5):513–517
Liaw KL, Hsing AW, Chen CJ, Schiffman MH, Zhang TY, Hsieh CY, Greer CE, You SL, Huang TW, Wu TC et al (1995) Human papillomavirus and cervical neoplasia: a case-control study in Taiwan. Int J Cancer 62:565–571
Matsukura T, Kanda T, Furuno A, Yoshikawa H, Kawana T, Yoshiike K (1986) Cloning of monomeric human papillomavirus type 16 DNA integrated within cell DNA from a cervical carcinoma. J Virol 58:979–982
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ, Meijer CJ (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348:518–527
Nagao S, Yoshinouchi M, Miyagi Y, Hongo A, Kodama J, Itoh S, Kudo T (2002) Rapid and sensitive detection of physical status of human papillomavirus type 16 DNA by quantitative real-time PCR. J Clin Microbiol 40:863–867
Nasiell K, Roger V, Nasiell M (1986) Behavior of mild cervical dysplasia during long-term follow-up. Obstet Gynecol 67:665–669
Park JS, Hwang ES, Park SN, Ahn HK, Um SJ, Kim CJ, Kim SJ, Namkoong SE (1997) Physical status and expression of HPV genes in cervical cancers. Gynecol Oncol 65:121–129
Pett MR, Herdman MT, Palmer RD, Yeo GS, Shivji MK, Stanley MA, Coleman N (2006) Selection of cervical keratinocytes containing integrated HPV16 associates with episome loss and an endogenous antiviral response. Proc Natl Acad Sci USA 103(10):3822–3827
Peitsaro P, Johansson B, Syrjanen S (2002) Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol 40:886–891
Pirami L, Giache V, Becciolini A (1997) Analysis of HPV16, 18, 31, and 35 DNA in pre-invasive and invasive lesions of the uterine cervix. J Clin Pathol 50:600–604
Soeda E, Ferran MC, Baker CC, McBride AA (2006) Repression of HPV16 early region transcription by the E2 protein. Virology 351(1):29–41
Schiffman MH, Bauer HM, Hoover RN, Glass AG, Cadell DM, Rush BB, Scott DR, Sherman ME, Kurman RJ, Wacholder S (1993) Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 85:958–964
Syrja¨nen K, Syrja¨nen S (2000) Papillomavirus infections. In: Human pathology. Wiley, Chichester, pp 1–615
Vizcaino AP, Moreno V, Bosch FX, Munoz N, Barros-Dios XM, Borras J, Parkin DM (2000) International trends in incidence of cervical cancer: II. Squamous-cell carcinoma. Int J Cancer 86:429–435
Wells SI, Francis DA, Karpova AY, Dowhanick JJ, Benson JD, Howley PM (2000) Papillomavirus E2 induces senescence in HPV-positive cells via pRB- and p21(CIP)-dependent pathways. Embo J 19:5762–5771
Werness BA, Levine AJ, Howley PM (1990) Association of human papilloma virus-16 and -18 E6 proteins with p53. Science 248:76–79
Wu S, Xu Q, Cheng G (2004) The comparative study on HPV DNA test for cervical scraping smears with PCR mediated by two different primers. Tumor 24:410–412
Yoshinouchi M, Hongo A, Nakamura K, Kodama J, Itoh S, Sakai H, Kudo T (1999) Analysis by multiplex PCR of the physical status of human papillomavirus type 16 DNA in cervical cancers. J Clin Microbiol 37:3514–3517
Zur Hausen H (1991) Human papillomaviruses in the pathogenesis of anogenital cancer. Virology 184:9–13
zur Hausen H (2000) Papillomaviruses causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst 92:690–698
Author information
Authors and Affiliations
Corresponding authors
Additional information
This study was supported by grants from the National Science Foundation of China (No. 30600667;30628029;30672227) and the “973” Program of China (No. 2002CB513100).
W. Li and W. Wang contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Li, W., Wang, W., Si, M. et al. The physical state of HPV16 infection and its clinical significance in cancer precursor lesion and cervical carcinoma. J Cancer Res Clin Oncol 134, 1355–1361 (2008). https://doi.org/10.1007/s00432-008-0413-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-008-0413-3