Abstract
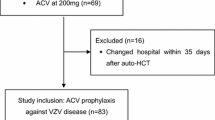
Varicella-zoster virus (VZV) reactivation is a relatively common cause of morbidity following autologous hematopoietic cell transplant (auto-HCT). The Centers for Disease Control in 2009 recommended extending VZV prophylaxis for 1 year post-transplantation. We retrospectively analyzed rates of VZV reactivation following auto-HCT at our transplant center prior to and after the implementation of extended antiviral prophylaxis in June 2008. The study population was divided into three different cohorts according to the length of VZV prophylaxis as following: (1) prophylaxis until neutrophil recovery to ≥500/μL (n = 77), (2) prophylaxis for 6 months (n = 12), or (3) 12 months (n = 40) post-auto-HCT. All patients received acyclovir 400 mg oral or intravenously twice daily or valacyclovir 500 mg oral daily. For patients in whom VZV reactivation occurred, data was collected on severity of infection, time of onset, treatment, and any associated complications. One hundred twenty-nine patients undergoing auto-HCT between January 1, 2004 and January 31, 2010 were included in the study. There was a significant difference in the rates of VZV reactivation between the neutrophil recovery and 12 months prophylaxis cohorts at 14 % (n = 11) and 2 % (n = 1) (P = 0.04), respectively. VZV reactivation rate in the 6-month prophylaxis group was 17 % (n = 2), but did not reach statistical significance due to small numbers. In the subset of auto-HCT patients treated with bortezomib, 13 % (n = 2) developed VZV reactivation in the neutrophil recovery group, while no events occurred in the other two cohorts. Complications of VZV reactivation include post-herpetic neuralgia (n = 5), severe pain (n = 3), scarring (n = 1), and motor weakness (n = 1); two patients required hospitalization and three patients developed disseminated zoster. Our limited retrospective analysis suggests a significant reduction in rates of post-auto-HCT rates of VZV reactivation with extended 12 months antiviral prophylaxis. VZV reactivation is a significant complication post-auto-HCT, and extended prophylaxis appears to be safe and effective in this setting.

Similar content being viewed by others
References
Su SH, Martel-Lafferriere V, Labbe A, Snydman DR, Kent D, Laverdiere M, et al. (2011) High incidence of herpes zoster in nonmyeloablative hematopoietic stem cell transplantation. Biol Blood Marrow Transplant [epub]:1–7
Shuchter LM, Wingard JR, Piantadosi S, Burns WH, Santos GW, Saral R (1989) Herpes zoster infection after autologous bone marrow transplantation. Blood 74(4):1424–1427
Sempere A, Sanz GF, Senent L, de la Rubia J, Jarque I, Lopez F et al (1992) Long-term acyclovir prophylaxis for prevention of varicella zoster virus infection after autologous blood stem cell transplantation in patients with acute leukemia. Bone Marrow Transplant 10:495–498
National Comprehensive Cancer Network Inc. Prevention and treatment of cancer-related infections. Version 1.2012. Available from http://www.nccn.org/professionals/physician_gls/PDF/infections.pdf. Accessed 15 Jan 2013
CDC, Infectious Disease Society of America, American Society of Blood and Marrow Transplantation (2000) Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients: recommendations of CDC, the Infectious Disease Society of America, and the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant 6(6a):659–713
Ljungman P, Wilczek H, Gahrton G, Gustavsson A, Lundgren G, Lönnqvist B et al (1986) Long term acyclovir prophylaxis in bone marrow transplant recipients and lymphocyte proliferation responses to herpes virus antigens in vitro. Bone Marrow Transplant 1:185–192
Erard V, Guthrie KA, Varley C, Heugel J, Wald A, Flowers ME et al (2007) One year acyclovir prophylaxis for preventing varicella zoster virus disease after hematopoietic cell transplantation: no evidence of rebound varicella-zoster virus disease after drug discontinuation. Blood 110(8):3071–3077
Channan-Khan A, Sonneveld P, Schuster MW, Stadtmauer EA, Facon T, Harousseau JL et al (2008) Analysis of herpes zoster events among bortezomib-treated patients in the phase III APEX study. J Clin Oncology 26(29):4784–4790
Center for Disease Control and Prevention. Available from http://www.cdc.gov/shingles/lab-testing/collecting-specimens.html. Accessed 15Jan 2013
Sampathkumar P, Drage LA, Martin DP (2009) Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 84(3):274–280
Onozawa M, Hashino S, Haseyama Y, Hirayama Y, Iizuka S, Ishida T et al (2009) Incidence and risk of postherpetic neuralgia after varicella zoster virus infection in hematopoietic cell transplantation recipients: Hokkaido Hematology Study Group. Biol Blood Marrow Transplant 15(6):724–729
Arvin AM (2000) Varicella-zoster virus: pathogenesis, immunity, and clinical management in hematopoietic cell transplant recipients. Biol Blood Marrow Transplant 6:219–230
Han CS, Miller W, Haake R, Weisdorf D (1994) Varicella zoster infection after bone marrow transplantation: incidence, risk factors and complications. Bone Marrow Transplant 13(3):277–283
Leung TF, Chik KW, Li CK, Lai H, Shing MM, Chan PK et al (2000) Incidence, risk factors and outcome of varicella-zoster virus infection in children after haematopoietic stem cell transplantation. Bone Marrow Transplant 25:167–172
Uy GL, Goyal SD, Fisher NM, Oza AY, Tomasson MH, Stockerl-Goldstein K et al (2009) Bortezomib administer pre-auto-SCT and as maintenance therapy post transplant for multiple myeloma: a single institution phase II study. Bone Marrow Transplant 43:793–800
Mateos MV, Hernández JM, Hernández MT, Gutiérrez NC, Palomera L, Fuertes M et al (2006) Bortezomib plus melphalan and prednisone in elderly untreated patients with multiple myeloma: results of a multicenter phase 1/2 study. Blood 108:2165–2172
Vickrey E, Allen S, Mehta J, Singhal S (2008) Acyclovir to prevent reactivation of varicella zoster virus (herpes zoster) in multiple myeloma patients receiving bortezomib therapy. Cancer 115:229–232
A Study to Evaluate the Safety and Efficacy of Inactivated Varicella-zoster Vaccine (VZV) as a Preventative Treatment for Herpes Zoster (HZ) and HZ-related Complications in Participants Undergoing Hematopoietic Cell Transplants (HCTs) (Study No. V212-001 AM4). Available from http://clinicaltrials.gov. Accessed 15 Jan 2013.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Truong, Q., Veltri, L., Kanate, A.S. et al. Impact of the duration of antiviral prophylaxis on rates of varicella-zoster virus reactivation disease in autologous hematopoietic cell transplantation recipients. Ann Hematol 93, 677–682 (2014). https://doi.org/10.1007/s00277-013-1913-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1913-z