Abstract
Purpose
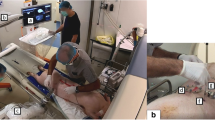
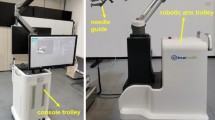
To compare CT fluoroscopy-guided manual and CT-guided robotic positioning system (RPS)-assisted needle placement by experienced IR physicians to targets in swine liver.
Materials and Methods
Manual and RPS-assisted needle placement was performed by six experienced IR physicians to four 5 mm fiducial seeds placed in swine liver (n = 6). Placement performance was assessed for placement accuracy, procedure time, number of confirmatory scans, needle manipulations, and procedure radiation dose. Intra-modality difference in performance for each physician was assessed using paired t test. Inter-physician performance variation for each modality was analyzed using Kruskal–Wallis test.
Results
Paired comparison of manual and RPS-assisted placements to a target by the same physician indicated accuracy outcomes was not statistically different (manual: 4.53 mm; RPS: 4.66 mm; p = 0.41), but manual placement resulted in higher total radiation dose (manual: 1075.77 mGy/cm; RPS: 636.4 mGy/cm; p = 0.03), required more confirmation scans (manual: 6.6; RPS: 1.6; p < 0.0001) and needle manipulations (manual: 4.6; RPS: 0.4; p < 0.0001). Procedure time for RPS was longer than manual placement (manual: 6.12 min; RPS: 9.7 min; p = 0.0003). Comparison of inter-physician performance during manual placement indicated significant differences in the time taken to complete placements (p = 0.008) and number of repositions (p = 0.04) but not in other study measures (p > 0.05). Comparison of inter-physician performance during RPS-assisted placement suggested statistically significant differences in procedure time (p = 0.02) and not in other study measures (p > 0.05).
Conclusions
CT-guided RPS-assisted needle placement reduced radiation dose, number of confirmatory scans, and needle manipulations when compared to manual needle placement by experienced IR physicians, with equivalent accuracy.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.





Similar content being viewed by others
References
Lu Y, Li C, Liu M et al (2013) MRI-guided stereotactic aspiration of brain abscesses by use of an optical tracking navigation system. Acta Radiol 55(1):121–128
Grasso RF, Cazzato RL, Luppi G et al (2013) Percutaneous lung biopsies: performance of an optical CT-based navigation system with a low-dose protocol. Eur Radiol 23(11):3071–3076
Ward TJ, Goldman RE, Weintraub JL (2013) Electromagnetic navigation with multimodality image fusion for image-guided percutaneous interventions. Tech Vasc Interv Radiol 16(3):177–181
Hakime A, Deschamps F, De Carvalho EG, Barah A, Auperin A, De Baere T (2012) Electromagnetic-tracked biopsy under ultrasound guidance: preliminary results. Cardiovasc Intervent Radiol 35(4):898–905
Banovac F, Cheng P, Campos-Nanez E et al (2010) Radiofrequency ablation of lung tumors in swine assisted by a navigation device with preprocedural volumetric planning. J Vasc Interv Radiol 21(1):122–129 2818540
Yeo CT, Ungi T, Lasso A, McGraw RC, Fichtinger G (2011) The effect of augmented reality training on percutaneous needle placement in spinal facet joint injections. IEEE Trans Biomed Eng 58(7):2031–2037
Neshat H, Cool DW, Barker K, Gardi L, Kakani N, Fenster A (2013) 3D ultrasound scanning system for image guided liver interventions. Med Phys 40(11):112903
Gao H, Luo CF, Hu CF, Zhang CQ, Zeng BF (2011) Minimally invasive fluoro-navigation screw fixation for the treatment of pelvic ring injuries. Surg Innov 18(3):279–284
Cleary K, Melzer A, Watson V, Kronreif G, Stoianovici D (2006) Interventional robotic systems: applications and technology state-of-the-art. Minim Invasive Ther Allied Technol 15(2):101–113
Fichtinger G, Fiene JP, Kennedy CW et al (2008) Robotic assistance for ultrasound-guided prostate brachytherapy. Med Image Anal 12(5):535–545
Onogi S, Morimoto K, Sakuma I et al (2005) Development of the needle insertion robot for percutaneous vertebroplasty. Med Image Comput Comput Assist Interv 8(Pt 2):105–113
Rasmus M, Huegli RW, Bilecen D, Jacob AL (2007) Robotically assisted CT-based procedures. Minim Invasive Ther Allied Technol 16(4):212–216
Zangos S, Melzer A, Eichler K et al (2011) MR-compatible assistance system for biopsy in a high-field-strength system: initial results in patients with suspicious prostate lesions. Radiology 259(3):903–910
Hungr N, Fouard C, Robert A, Bricault I, Cinquin P (2011) Interventional radiology robot for CT and MRI guided percutaneous interventions. Med Image Comput Comput Assist Interv 14(Pt 1):137–144
Koethe Y, Xu S, Velusamy G, Wood BJ, Venkatesan AM (2013) Accuracy and efficacy of percutaneous biopsy and ablation using robotic assistance under computed tomography guidance: a phantom study. Eur Radiol 24(3):723–730
Patriciu A, Awad M, Solomon SB et al (2005) Robotic assisted radio-frequency ablation of liver tumors–randomized patient study. Med Image Comput Comput Assist Interv 8(Pt 2):526–533
Stoffner R, Augscholl C, Widmann G, Bohler D, Bale R (2009) Accuracy and feasibility of frameless stereotactic and robot-assisted CT-based puncture in interventional radiology: a comparative phantom study. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 181(9):851–858
Schulz B, Eichler K, Siebenhandl P et al (2013) Accuracy and speed of robotic assisted needle interventions using a modern cone beam computed tomography intervention suite: a phantom study. Eur Radiol 23(1):198–204
Schell B, Eichler K, Mack MG et al (2012) Robot-assisted biopsies in a high-field MRI system—first clinical results. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 184(1):42–47
Mozer P, Troccaz J, Stoianovici D (2009) Urologic robots and future directions. Curr Opin Urol 19(1):114–119
Solomon SB, Patriciu A, Bohlman ME, Kavoussi LR, Stoianovici D (2002) Robotically driven interventions: a method of using CT fluoroscopy without radiation exposure to the physician. Radiology 225(1):277–282 3107539
Gianfelice D, Lepanto L, Perreault P, Chartrand-Lefebvre C, Milette PC (2000) Effect of the learning process on procedure times and radiation exposure for CT fluoroscopy-guided percutaneous biopsy procedures. J Vasc Interv Radiol 11(9):1217–1221
Silverman SG, Tuncali K, Adams DF, Nawfel RD, Zou KH, Judy PF (1999) CT fluoroscopy-guided abdominal interventions: techniques, results, and radiation exposure. Radiology 212(3):673–681
Tovar-Arriaga S, Tita R, Pedraza-Ortega JC, Gorrostieta E, Kalender WA (2011) Development of a robotic FD-CT-guided navigation system for needle placement-preliminary accuracy tests. Int J Med Robot Comput Assist Surg 7(2):225–236
Yanof J, Haaga J, Klahr P et al (2001) CT-integrated robot for interventional procedures: preliminary experiment and computer-human interfaces. Comput Aided Surg 6(6):352–359
Abdullah BJ, Yeong CH, Goh KL et al (2014) Robot-assisted radiofrequency ablation of primary and secondary liver tumours: early experience. Eur Radiol 24(1):79–85
Zhou Y, Thiruvalluvan K, Krzeminski L, Moore WH, Xu Z, Liang Z (2013) CT-guided robotic needle biopsy of lung nodules with respiratory motion—experimental system and preliminary test. Int J Med Robot 9(3):317–330
Pollock R, Mozer P, Guzzo TJ et al (2010) Prospects in percutaneous ablative targeting: comparison of a computer-assisted navigation system and the AcuBot robotic system. J Endourol 24(8):1269–1272
Bax JS, Waring CS, Sherebrin S et al (2013) 3D image-guided robotic needle positioning system for small animal interventions. Med Phys 40(1):011909
Nawfel RD, Judy PF, Silverman SG, Hooton S, Tuncali K, Adams DF (2000) Patient and personnel exposure during CT fluoroscopy-guided interventional procedures. Radiology 216(1):180–184
Kato R, Katada K, Anno H, Suzuki S, Ida Y, Koga S (1996) Radiation dosimetry at CT fluoroscopy: physician’s hand dose and development of needle holders. Radiology 201(2):576–578
Nickoloff EL, Khandji A, Dutta A (2000) Radiation doses during CT fluoroscopy. Health Phys 79(6):675–681
Daly B, Krebs TL, Wong-You-Cheong JJ, Wang SS (1999) Percutaneous abdominal and pelvic interventional procedures using CT fluoroscopy guidance. AJR Am J Roentgenol 173(3):637–644
Paulson EK, Sheafor DH, Enterline DS, McAdams HP, Yoshizumi TT (2001) CT fluoroscopy–guided interventional procedures: techniques and radiation dose to radiologists. Radiology 220(1):161–167
Baek SK, Carmichael JC, Pigazzi A (2013) Robotic surgery: colon and rectum. Cancer J 19(2):140–146
Evans SM, Millar JL, Frydenberg M et al (2014) Positive surgical margins: rate, contributing factors and impact on further treatment: findings from the Prostate Cancer Registry. BJU Int 114(5):680–690
Oggero E, Pagnacco G, Morr DR, Barnes SZ, Berme N (1997) The mechanics of drop landing on a flat surface—a preliminary study. Biomed Sci Instrum 33:53–58
Baur C, Guzzoni D, Georg O (1998) VIRGY: a virtual reality and force feedback based endoscopic surgery simulator. Stud Health Technol Inform 50:110–116
Tiong L, Maddern GJ (2011) Systematic review and meta-analysis of survival and disease recurrence after radiofrequency ablation for hepatocellular carcinoma. Br J Surg 98(9):1210–1224
Kobayashi K, Bhargava P, Raja S et al (2012) Image-guided biopsy: what the interventional radiologist needs to know about PET/CT. Radiographics 32(5):1483–1501
Hui GC, Tuncali K, Tatli S, Morrison PR, Silverman SG (2008) Comparison of percutaneous and surgical approaches to renal tumor ablation: metaanalysis of effectiveness and complication rates. J Vasc Interv Radiol 19(9):1311–1320
Acknowledgments
F. Cornelis would like to acknowledge support from CHU de Bordeaux, Université de Bordeaux, Canceropôle du Grand Sud-Ouest, Association de la Recherche contre le Cancer, Société Française de Radiologie, Société d’Imagerie Génito-Urinaire, Philippe Foundation and the Fulbright Scholarship Program.
Conflict of interest
The project was performed with support of a grant to the corresponding author (GS) from Perfint Healthcare Inc. The grant provided salary support for GS for performing the study. The others have no conflict of interest to report. Author #3 (ML) is a salaried employee of Perfint Healthcare Inc who provided technical support with the robot positioning system for the duration of the experiments. ML was not involved in the design of experiments, data collection, analysis, or interpretation of presented results.
Statement of Human and Animal Rights
The study has been approved by the appropriate institutional research ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cornelis, F., Takaki, H., Laskhmanan, M. et al. Comparison of CT Fluoroscopy-Guided Manual and CT-Guided Robotic Positioning System for In Vivo Needle Placements in Swine Liver. Cardiovasc Intervent Radiol 38, 1252–1260 (2015). https://doi.org/10.1007/s00270-014-1016-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-014-1016-9