Abstract
Purpose
Periprosthetic joint infections remain a major challenge for the surgeon in modern arthroplasty. The decision on how to handle a case is often difficult due to the variety of clinical presentations. The aim of this study was to establish the leucocyte esterase test as an intra-operative rapid diagnostic tool in an unclear infected or aseptic situation.
Methods
In the setting of 364 endoprosthetic joint procedures on knee, hip and shoulder, we aspirated synovial fluid before performing capsulotomy. We performed a leucocyte esterase test. The results were correlated with the pre-operative synovial fluid aspirations, the laboratory blood sample parameters (C-reactive protein, white blood cells) and the intra-operative histopathological and microbiological findings.
Results
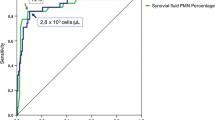
The leucocyte esterase test has a sensitivity of 100 % and a specificity of 96.5 %. The positive predictive value was 82 % and the negative predictive value was 100 %. Correlation with conventional methods such as serum C-reactive protein and serum white blood cells is given. The histopathological evaluation confirmed the microbiological results in all but three cases.
Conclusions
Based on our results and the current literature, we recommend the leucocyte esterase test as a useful tool in the diagnosis of periprosthetic joint infection.



Similar content being viewed by others
References
Peel TN, Dowsey MM, Buising KL, Liew D, Choong PF (2013) Cost analysis of debridement and retention for management of prosthetic joint infection. Clin Microbiol Infect 19(2):181–186. doi:10.1111/j.1469-0691.2011.03758.x
Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J (2013) Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg Am 95(24):2177–2184. doi:10.2106/JBJS.L.00789
Klouche S, Sariali E, Mamoudy P (2010) Total hip arthroplasty revision due to infection: a cost analysis approach. Orthop Traumatol Surg Res 96(2):124–132. doi:10.1016/j.rcot.2010.02.005
Parvizi J, Adeli B, Zmistowski B, Restrepo C, Greenwald AS (2012) Management of periprosthetic joint infection: the current knowledge: AAOS exhibit selection. J Bone Joint Surg Am 94(14):e104. doi:10.2106/JBJS.K.01417
Duff GP, Lachiewicz PF, Kelley SS (1996) Aspiration of the knee joint before revision arthroplasty. Clin Orthop Relat Res 331:132–139
Parvizi J, Jacovides C, Antoci V, Ghanem E (2011) Diagnosis of periprosthetic joint infection: the utility of a simple yet unappreciated enzyme. J Bone Joint Surg Am 93(24):2242–2248. doi:10.2106/JBJS.J.01413
St John A, Boyd JC, Lowes AJ, Price CP (2006) The use of urinary dipstick tests to exclude urinary tract infection: a systematic review of the literature. Am J Clin Pathol 126(3):428–436. doi:10.1309/C69RW1BT7E4QAFPV
Smalley DL, Dittmann AN (1983) Use of leukocyte esterase-nitrate activity as predictive assays of significant bacteriuria. J Clin Microbiol 18(5):1256–1257
Koulaouzidis A, Leontiadis GI, Abdullah M, Moschos J, Gasem J, Tharakan J, Maltezos E, Saeed AA (2008) Leucocyte esterase reagent strips for the diagnosis of spontaneous bacterial peritonitis: a systematic review. Eur J Gastroenterol Hepatol 20(11):1055–1060. doi:10.1097/MEG.0b013e328300a363
Hurley RM, Wright DW, Wilson GW, Ali MA (1981) Detection of leucocytes in peritoneal effluent by test strip. Lancet 1(8217):437–438
Azoulay E, Fartoukh M, Galliot R, Baud F, Simonneau G, Le Gall JR, Schlemmer B, Chevret S (2000) Rapid diagnosis of infectious pleural effusions by use of reagent strips. Clin Infect Dis 31(4):914–919. doi:10.1086/318140
Lebovics RS, Murthy VV, Karmen A (1993) Leukocyte esterase activity in effusion fluid of patients with otitis media. Otolaryngol Head Neck Surg 108(3):248–250
Morawietz L, Classen RA, Schröder JH, Dynybil C, Perka C, Skwara A, Neidel J, Gehrke T, Frommelt L, Hansen T, Otto M, Barden B, Aigner T, Stiehl P, Schubert T, Meyer-Scholten C, König A, Ströbel P, Rader CP, Kirschner S, Lintner F, Rüther W, Bos I, Hendrich C, Kriegsmann J, Krenn V (2006) Proposal for a histopathological consensus classification of the periprosthetic interface membrane. J Clin Pathol 59(6):591–597. doi:10.1136/jcp.2005.027458
Browne JA, Bechtold CD, Berry DJ, Hanssen AD, Lewallen DG (2010) Failed metal-on-metal hip arthroplasties: a spectrum of clinical presentations and operative findings. Clin Orthop Relat Res 468(9):2313–2320. doi:10.1007/s11999-010-1419-0
Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valle CJ (2012) Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J Arthroplasty 27(8 Suppl):8–11. doi:10.1016/j.arth.2012.03.037
Aggarwal VK, Tischler E, Ghanem E, Parvizi J (2013) Leukocyte esterase from synovial fluid aspirate: a technical note. J Arthroplasty 28(1):193–195. doi:10.1016/j.arth.2012.06.023
Günther R, Morawietz L, Gehrke T, Frommelt L, Kaps C, Krenn V (2005) Inflammatory reactions in the wear particle induced and infectious periprosthetic membrane of loosened hip- and knee endoprostheses: pathogenetic relevance of differentially expressed genes cd9, cd11b, cd18, cd52 and pdgfrbeta. Orthopade 34(1):55–64. doi:10.1007/s00132-004-0709-1
Willert HG, Semlitsch M (1977) Reactions of the articular capsule to wear products of artificial joint prostheses. J Biomed Mater Res 11(2):157–164. doi:10.1002/jbm.820110202
Corona P, Gil E, Guerra E, Soldado F, Amat C, Flores X, Pigrau C (2012) Percutaneous interface biopsy in dry-aspiration cases of chronic periprosthetic joint infections: a technique for preoperative isolation of the infecting organism. Int Orthop 36(6):1281–1286. doi:10.1007/s00264-011-1418-0
Zmistowski B, Restrepo C, Huang R, Hozack WJ, Parvizi J (2012) Periprosthetic joint infection diagnosis: a complete understanding of white blood cell count and differential. J Arthroplasty 27(9):1589–1593. doi:10.1016/j.arth.2012.03.059
Toossi N, Adeli B, Rasouli MR, Huang R, Parvizi J (2012) Serum white blood cell count and differential do not have a role in the diagnosis of periprosthetic joint infection. J Arthroplasty 27(8):51–54. doi:10.1016/j.arth.2012.03.021
Ghanem E, Antoci V Jr, Pulido L, Joshi A, Hozack W, Parvizi J (2009) The use of receiver operating characteristics analysis in determining erythrocyte sedimentation rate and C-reactive protein levels in diagnosing periprosthetic infection prior to revision total hip arthroplasty. Int J Infect Dis 13(6):e444–e449. doi:10.1016/j.ijid.2009.02.017
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J 95-B(11):1450–1452. doi:10.1302/0301-620X.95B11.33135
Johnson AJ, Zywiel MG, Stroh A, Marker DR, Mont MA (2011) Serological markers can lead to false negative diagnoses of periprosthetic infections following total knee arthroplasty. Int Orthop 35(11):1621–1626. doi:10.1007/s00264-010-1175-5
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469(11):2992–2994. doi:10.1007/s11999-011-2102-9
Kelly EG, Cashman JP (2013) Leucocyte esterase in the rapid diagnosis of paediatric septic arthritis. Med Hypotheses 80(2):191–193. doi:10.1016/j.mehy.2012.11.026
Parvizi J, McKenzie JC, Cashman JP (2012) Diagnosis of periprosthetic joint infection using synovial C-reactive protein. J Arthroplasty 27(8 Suppl):12–16. doi:10.1016/j.arth.2012.03.018
Yi PH, Cross MB, Moric M, Sporer SM, Berger RA, Della Valle CJ (2014) The 2013 Frank Stinchfield Award: diagnosis of infection in the early postoperative period after total hip arthroplasty. Clin Orthop Relat Res 472(2):424–429. doi:10.1007/s11999-013-3089-1
Tsaras G, Maduka-Ezeh A, Inwards CY, Mabry T, Erwin PJ, Murad MH, Montori VM, West CP, Osmon DR, Berbari EF (2012) Utility of intraoperative frozen section histopathology in the diagnosis of periprosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am 94(18):1700–1711. doi:10.2106/JBJS.J.00756
Acknowledgments
This study was supported by HELIOS Kliniken GmbH, grant ID 004145. Major parts of this contribution are components of the thesis of Thomas Kokenge.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guenther, D., Kokenge, T., Jacobs, O. et al. Excluding infections in arthroplasty using leucocyte esterase test. International Orthopaedics (SICOT) 38, 2385–2390 (2014). https://doi.org/10.1007/s00264-014-2449-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2449-0