Abstract
Introduction
Inflammation-based scoring systems have potential value in evaluating the prognosis of cancer patients; however, detailed comparative analyses in well-characterized head and neck cancer patient collectives are missing.
Methods
We analyzed overall survival (OS) in locally advanced head and neck cancer patients who were treated with curative intent by primary radiotherapy (RT) alone, by RT in combination with cetuximab (RIT) or with cisplatin (RCHT), and by primary surgery followed by postoperative radiotherapy (PORT). The primary RT collective (N = 170) was analyzed separately from the surgery plus RT group (N = 148). OS was estimated using the Kaplan–Meyer method. Cox proportional-hazard regression models were applied to compare the risk of death among patients stratified according to risk factors and the inflammation-based Glasgow Prognostic Score (GPS), the modified GPS (mGPS), the neutrophil–lymphocyte ratio (NLR), the platelet–lymphocyte ratio (PLR), and the prognostic index (PI).
Results
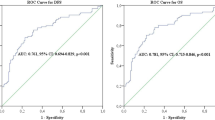
A prognostic relevance of the scoring systems for OS was observed in the primarily irradiated, but not in the PORT collective. OS was 35.5, 18.8, and 15.4 months, respectively, according to GPS 0, 1, and 2. OS according to mGPS 0–2 was identical. The PLR scoring system was not of prognostic relevance, while OS was 27.3 months in the NLR 0 group and 17.3 months in the NLR 1 group. OS was 35.5 months in PI 0, 16.1 months in PI 1, and 22.6 months in PI 2.
Conclusion
GPS/mGPS scoring systems are able to discriminate between three risk groups in primarily, but not postoperatively irradiated locally advanced head and neck cancer patients.
Zusammenfassung
Hintergrund
Entzündungsbasierte Bewertungssysteme haben eine potenzielle Bedeutung für die Beurteilung der Prognose von Krebspatienten. Derzeit fehlen jedoch ausreichend detailliert durchgeführte Analysen in Kollektiven von Patienten mit Kopf-Hals-Tumoren.
Methoden
Untersucht wurde das Gesamtüberleben („overall survival“, OS) von Patienten mit lokal fortgeschrittenen Kopf-Hals-Tumoren, die in kurativer Intention mit einer alleinigen primären Radiotherapie (RT), mit RT in Kombination mit Cetuximab (RIT) oder Cisplatin (RCHT) sowie mittels primärer Chirurgie gefolgt von postoperativer RT (PORT) behandelt wurden. Patienten, die primär radiotherapiert wurden (N = 170), wurden getrennt vom PORT-Kollektiv (N = 148) analysiert. OS wurde mittels der Kaplan-Meier-Methode ermittelt. Cox-proportionale Hazard-Regressionsmodelle wurden eingesetzt, um das Sterberisiko, stratifiziert nach Risikofaktoren und dem entzündungsbasierten Glasgow-Prognosescore (GPS), dem modifizierten GPS (mGPS), der Neutrophilen-Lymphozyten-Ratio (NLR), der Thrombozyten-Lymphozyten-Ratio (PLR) und dem Prognoseindex (PI) zu vergleichen.
Ergebnisse
Eine prognostische Bedeutung der untersuchten Bewertungssysteme wurde nur in der primär bestrahlten Patientengruppe, jedoch nicht im PORT-Kollektiv gefunden. Das Gesamtüberleben in GPS 0, 1 und 2 betrug jeweils 35,5, 18,8 und 15,4 Monate. Das Gesamtüberleben nach mGPS war in allen Gruppen identisch. Das PLR-Bewertungssystem hatte keine prognostische Relevanz, während das Gesamtüberleben in der NLR-0-Gruppe 27,3 und in der NLR-1-Gruppe 17,3 Monate betrug. Das Gesamtüberleben in PI 0 betrug 35,5, in PI 1 16,1 und in PI 2 22,6 Monate.
Schlussfolgerung
Die GPS/mGPS-Bewertungssysteme können bei primär, jedoch nicht bei postoperativ bestrahlten lokal fortgeschrittenen Kopf-Hals-Tumorpatienten zwischen 3 verschiedenen Risikogruppen diskriminieren.

Similar content being viewed by others
References
An X, Ding PR, Wang FH, Jiang WQ, Li YH (2011) Elevated neutrophil to lymphocyte ratio predicts poor prognosis in nasopharyngeal carcinoma. Tumour Biol 32:317–324
Ang KK, Harris J, Wheeler R et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363:24–35
Azab B, Shah N, Radbel J, Tan P, Bhatt V, Vonfrolio S, Habeshy A, Picon A, Bloom S (2013) Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients. Med Oncol 30:432
Azab B, Shariff MA, Bachir R, Nabagiez JP, McGinn JT Jr (2013) Elevated preoperative neutrophil/lymphocyte ratio as a predictor of increased long-term survival in minimal invasive coronary artery bypass surgery compared to sternotomy. J Cardiothorac Surg 8:193
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Colotta F, Allavena P, Sica A et al (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 7:1073–1081
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Curry JM, Sprandio J, Cognetti D, Luginbuhl A, Bar-Ad V, Pribitkin E, Tuluc M (2014) Tumor microenvironment in head and neck squamous cell carcinoma. Semin Oncol 41:217–234
Fang HY, Huang XY, Chien HT, Chang JT, Liao CT, Huang JJ, Wei FC, Wang HM, Chen IH, Kang CJ, Huang SF (2013) Refining the role of preoperative C-reactive protein by neutrophil/lymphocyte ratio in oral cavity squamous cell carcinoma. Laryngoscope 123:2690–2699
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ (2003) Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small cell lung cancer. Br J Cancer 89:1028–1030
Gabay C, Kuschner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:1376
Grimm M, Lazariotou M (2012) Clinical relevance of a new pre-treatment laboratory prognostic index in patients with oral squamous cell carcinoma. Med Oncol 29:1435–47
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674 (Review)
Hanahan D, Coussens LM (2012) Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell 21:309–322 (Review)
He JR, Shen GP, Ren ZF, Qin H, Cui C, Zhang Y et al (2012) Pretreatment levels of peripheral neutrophils and lymphocytes as independent prognostic factors in patients with nasopharyngeal carcinoma. Head Neck 34:1769–1776
Khandavilli SD, Ceallaigh PO, Lloyd CJ, Whitaker R (2009) Serum C-reactive protein as a prognostic indicator in patients with oral squamous cell carcinoma. Oral Oncol 45:912–914
McMillan DC (2008) An inflammation-based prognostic score and its role in the nutrition based management of patients with cancer. Proc Nutr Soc 67:257–262
McMillan DC (2013) The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev 39:534–540 (Review)
Millrud CR, Månsson Kvarnhammar A, Uddman R, Björnsson S, Riesbeck K, Cardell LO (2012) The activation pattern of blood leukocytes in head and neck squamous cell carcinoma is correlated to survival. PLoS One 7:e51120
Heiduschka G, Grah A, Oberndorfer F, Kadletz L, Altorjai G, Kornek G, Wrba F, Thurnher D, Selzer E (2014). Improved survival in HPV/p16-positive oropharyngeal cancer patients treated with postoperative radiotherapy. Strahlenther Onkol. 2014 Sep 25. [Epub ahead of print].
Heiduschka G, Grah A, Oberndorfer F, Seemann R, Kranz A, Kornek G, Wrba F, Thurnher D, Selzer E (2014). Significance of p16 expression in head and neck cancer patients treated with radiotherapy and cetuximab. Strahlenther Onkol 190:832–8.
Perisanidis C, Kornek G, Pöschl PW, Holzinger D, Pirklbauer K, Schopper C, Ewers R (2013) High neutrophil-to-lymphocyte ratio is an independent marker of poor disease-specific survival in patients with oral cancer. Med Oncol 30:334
Proctor MJ, Talwar D, Balmar SM, O’Reilly DS, Foulis AK, Horgan PG, Morrison DS, McMillan DC (2010) The relationship between the presence and site of cancer, an inflammation-based prognostic score and biochemical parameters. Initial results of the Glasgow Inflammation Outcome Study. Br J Cancer 103:870–876
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47:2633–2641
Rades D, Seibold ND, Gebhard MP, Noack F, Schild SE, Thorns C (2013) Prognostic factors (including HPV status) for irradiation of locally advanced squamous cell carcinoma of the head and neck (SCCHN). Strahlenther Onkol 187:626–632
Roxburgh CS, McMillan DC (2010) Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 6:149–163 (Review)
Rutkowski T, Wygoda A, Składowski K, Hejduk B, Rutkowski R, Kołosza Z, Maciejewski B (2013) Prognostic role of tumor volume for radiotherapy outcome in patient with T2 laryngeal cancer. Strahlenther Onkol 189:861–866
Sadat F, Wienke A, Dunst J, Kuhnt T (2012) Survival of patients with head and neck cancer. Impact of physical status and comorbidities. Strahlenther Onkol 188:62–70
Stockmann C, Schadendorf D, Klose R, Helfrich I (2014) The impact of the immune system on tumor: angiogenesis and vascular remodeling. Front Oncol 4:69 (Review)
Tlsty TD, Coussens LM (2006) Tumor stroma and regulation of cancer development. Annu Rev Pathol 1:119–150
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
E. Selzer, A. Grah, G. Heiduschka, G, Kornek, and D. Thurnher state that there are no conflicts of interest.
The accompanying manuscript does not include studies on humans or animals.
Additional information
E.S. and A.G. should be regarded as equal contributors.
Rights and permissions
About this article
Cite this article
Selzer, E., Grah, A., Heiduschka, G. et al. Primary radiotherapy or postoperative radiotherapy in patients with head and neck cancer. Strahlenther Onkol 191, 486–494 (2015). https://doi.org/10.1007/s00066-014-0803-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0803-1