Abstract
Background and Purpose
Local control of metastatic spinal cord compression (MSCC) is particularly important for long-term survivors. Radiotherapy alone is the most common treatment for MSCC. The most frequently used schedule world wide is 30 Gy/10 fractions. This study investigated whether patients with favorable survival prognoses benefit from a dose escalation beyond 30 Gy.
Patients and Methods
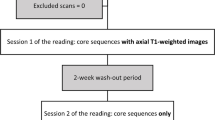
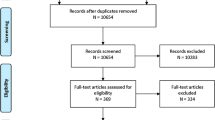
Data from 191 patients treated with 30 Gy/10 fractions were matched to 191 patients (1:1) receiving higher doses (37.5 Gy/15 fractions or 40 Gy/20 fractions). All patients had favorable survival prognoses based on a validated scoring system and were matched for age, gender, tumor type, performance status, number of involved vertebrae, visceral or other bone metastases, interval from tumor diagnosis to radiotherapy, ambulatory status, and time developing motor deficits. Both groups were compared for local control, progression-free survival, overall survival, and functional outcome.
Results
Local control rates at 2 years were 71 % after 30 Gy and 92 % after higher doses (p = 0.012). Two-year progression-free survival rates were 68 % and 90 %, respectively (p = 0.013). Two-year overall survival rates were 53 % and 68 %, respectively (p = 0.032). Results maintained significance in the multivariate analyses (Cox proportional hazards model; stratified model) with respect to local control (p = 0.011; p = 0.012), progression-free survival (p = 0.010; p = 0.018), and overall survival (p = 0.014; p = 0.015). Functional outcome was similar in both groups. Motor function improved in 40 % of patients after 30 Gy and 41 % after higher doses (p = 0.98).
Conclusion
Escalation of the radiation dose beyond 30 Gy resulted in significantly better local control, progression-free survival, and overall survival in patients with favorable survival prognoses.
Zusammenfassung
Hintergrund
Die lokale Kontrolle der metastatisch bedingten Rückenmarkkompression (MSCC) ist von besonderer Bedeutung für Patienten mit vergleichsweise guter Überlebensprognose. Die alleinige Strahlentherapie ist die häufigste Behandlungsform der MSCC; das am meisten verwendete Fraktionierungsschema ist 30 Gy/10 Fraktionen. Diese Studie untersuchte, ob Patienten mit vergleichsweise guter Überlebensprognose von einer Dosiseskalation über 30 Gy hinaus profitieren.
Patienten und Methoden
191 Patienten, die 30 Gy/10 Fraktionen erhielten, wurden mit 191 Patienten, die höhere Dosen (37,5 Gy/15 Fraktionen oder 40 Gy/20 Fraktionen) erhielten, verglichen (Matched-Pair-Analyse). Alle Patienten hatten nach einem validierten Score eine vergleichsweise gute Überlebensprognose. Die Paarbildung erfolgte unter Berücksichtigung folgender Faktoren: Alter, Geschlecht, Art des Primärtumors, Allgemeinzustand, Anzahl betroffener Wirbelkörper, viszerale Metastasen, weitere Knochenmetastasen, Intervall von der Erstdiagnose der Tumorerkrankung bis zur Bestrahlung, Gehfähigkeit, Entwicklungszeit motorischer Defizite. Beide Grupen wurden hinsichtlich lokaler Kontrolle, progressionsfreiem Überleben, Gesamtüberleben und motorischer Funktion verglichen.
Ergebnisse
Die Raten für die lokale Kontrolle nach 2 Jahren betrugen 71 % nach 30 Gy und 92 % nach höheren Dosen (p = 0,012). Die Raten für das progressionsfreie Überleben waren 68 % und 90 % (p = 0,013), die Raten für das Gesamtüberleben 53 % und 68 % (p = 0,032). Die Ergebnisse blieben in den Multivarianzanalysen (Cox proportional hazards model; stratified model) signifikant für die lokale Kontrolle (p = 0,011; p = 0,012), das progressionsfreie Überleben (p = 0,010; p = 0,018) und das Gesamtüberleben (p = 0,014; p = 0,015). Eine Verbesserung der motorischen Funktion war bei 40 % der Patienten nach 30 Gy und bei 41 % nach höheren Dosen zu verzeichnen (p = 0,98).
Schlussfolgerung
Eine Dosiseskalation über 30 Gy hinaus führt zu einer signifikanten Verbesserung von lokaler Kontrolle, progressionsfreiem Überleben und Gesamtüberleben.
Similar content being viewed by others
References
Freundt K, Meyners T, Bajrovic A et al. Radiotherapy for oligometastatic disease in patients with spinal cord compression (MSCC) from relatively radioresistant tumors. Strahlenther Onkol 2010;186:218–23.
Gerszten PC, Burton SA, Ozhasoglu C et al. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine 2007;32:193–9.
Joiner MC, Van der Kogel AJ. The linear-quadratic approach to fractionation and calculation of isoeffect relationships. In: Steel GG (ed) Basic clinical radiobiology. New York, Oxford University Press, 1997, pp 106–12.
Kaplan EL, Meier P. Non parametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–81.
Milker-Zabel S, Zabel A, Thilmann C et al. Clinical results of retreatment of vertebral bone metastases by stereotactic conformal radiotherapy and intensity- modulated radiotherapy. Int J Radiat Oncol Biol Phys 2003;55:162–7.
Mirri MA, Arcangeli G, Benassi M et al. Hypofractionated conformal radiotherapy (HCRT) for primary and metastatic lung cancers with small dimension: efficacy and toxicity. Strahlenther Onkol 2009;185:27–33.
Nieder C, Haukland E, Pawinski A et al. Validation of new prognostic and predictive scores by sequential testing approach. Strahlenther Onkol 2010, Feb 22 [Epub ahead of print].
Patchell R, Tibbs PA, Regine WF et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005;366:643–8.
Prasad D, Schiff D. Malignant spinal cord compression. Lancet Oncol 2005;6:15–24.
Quinn JA, DeAngelis LM. Neurologic emergencies in the cancer patient. Semin Oncol 2000;27:311–21.
Rades D, Dunst J, Schild SE. The first score predicting overall survival in patients with metastatic spinal cord compression. Cancer 2008;112:157–61.
Rades D, Huttenlocher S, Dunst J et al. Matched pair analysis comparing surgery followed by radiotherapy and radiotherapy alone for metastatic spinal cord compression. J Clin Oncol 2010;28:3597–604.
Rades D, Karstens JH, Hoskin PJ et al. Escalation of radiation dose beyond 30 Gy in 10 fractions for metastatic spinal cord compression. Int J Radiat Oncol Biol Phys 2007;67:525–31.
Rades D, Lange M, Veninga T et al. Preliminary results of spinal cord compression recurrence evaluation (SCORE-1) study comparing short-course versus long-course radiotherapy for local control of malignant epidural spinal cord compression. Int J Radiat Oncol Biol Phys 2009;73:228–34.
Rades D, Stalpers LJA, Veninga T et al. Evaluation of five radiation schedules and prognostic factors for metastatic spinal cord compression in a series of 1304 patients. J Clin Oncol 2005;23:3366–75.
Souchon R, Wenz F, Sedlmayer F et al. DEGRO practice guidelines for palliative radiotherapy of metastatic breast cancer: bone metastases and metastatic spinal cord compression. Strahlenther Onkol 2009;185:417–24.
Tomita T, Galicich JH, Sundaresan N. Radiation therapy for spinal epidural metastases with complete block. Acta Radiol Oncol 1983;22:135–43.
Trotti A, Byhardt R, Stetz J et al. Common toxicity criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:13–47.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rades, D., Panzner, A., Rudat, V. et al. Dose escalation of radiotherapy for Metastatic Spinal Cord Compression (MSCC) in patients with relatively favorable survival prognosis. Strahlenther Onkol 187, 729–735 (2011). https://doi.org/10.1007/s00066-011-2266-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-011-2266-y